BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-2283-en.html

 , Davood Farzin2
, Davood Farzin2 

 , Samaneh Farrokhfar3
, Samaneh Farrokhfar3 

 , Erfan Darban Razavi1
, Erfan Darban Razavi1 

 , Alireza Vahdatinia4
, Alireza Vahdatinia4 

 , Parnian Azadtarigheh5
, Parnian Azadtarigheh5 

 , Bahareh Lashtoo Aghaee6
, Bahareh Lashtoo Aghaee6 


2- Department of Pharmacology, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
3- Department of Anatomical Sciences, Faculty of Medicine, Ramsar Campus, Mazandaran University of Medical Sciences, Ramsar, Iran
4- Student Research Committee, Mazandaran University of Medical Sciences Faculty of Medicine, Sari, Iran
5- Department of Medicine, Faculty of Medicine, Ramsar Campus, Mazandaran University of Medical Sciences, Ramsar, Iran
6- Department of Microbiology, Faculty of Medicine, Ramsar Campus, Mazandaran University of Medical Sciences, Ramsar, Iran ,
Annually, over 1.27 million global deaths are attributed to antibiotic-resistant bacterial infections, with 35,000 individuals succumbing to the consequences of 2.8 million infections in the United States alone (1,2). The World Health Organization (WHO) has emphasized the urgent need for novel antibiotics to combat infections caused by carbapenem-resistant Pseudomonas aeruginosa, ranking it among the top three bacterial threats of infections (3). Pseudomonas aeruginosa is a significant cause of nosocomial infections, particularly in the intensive care unit (ICU), resulting in increased morbidity and mortality, impacting patients with cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD), and hospital-acquired pneumonia (4).
In response to the escalating antibiotic resistance crisis, the WHO has identified 12 antibiotic-resistant bacterial species as critical threats to human health, with P. aeruginosa serving as a prominent source of healthcare-associated infections (HAIs), notably in severe burn cases (5). Risk factors for Pseudomonas infections in burn patients encompass factors such as the extent of burnt body surface area, presence of P. aeruginosa in the clinical environment, previous use of broad-spectrum antibiotics like carbapenems, and a prolonged hospital stay (6). Management of suspected P. aeruginosa infections in burnt patients entails initiating antibiotic treatment and collecting cultures, especially in severe cases admittance to the ICU ward. Surveillance such as source control is pivotal, This involves the removal of potential P. aeruginosa sources like catheters artificial respiratory devices, and nebulizers (7). In severe cases, surgical intervention, including debridement of necrotic tissue, is a viable source control strategy (6). Conversely, mild cases often warrant topical agents as the primary treatment approach.
Among the antimicrobial agents, silver Sulfadiazine and mafenide acetate topical creams exhibit broad-spectrum activity against both gram-positive and gram-negative bacteria (8). In cases of adverse drug reactions, bacitracin and mupirocin ointments are considered as an alternative (9). Additionally, certain plant species, including Arnebia euchroma (Abukhalsa ointment), Aloe vera, and Actinidia deliciosa, have demonstrated to have a high efficacy in burn wound healing (10).
The increasing prevalence of antibiotic-resistant P. aeruginosa strains in healthcare-associated infections, in combination with the decline in the development of new antibiotics, has spurred researchers to explore alternative treatments. Bacteriophages, often referred to as "phages," offer a promising alternative. These natural bacterial controllers are abundant and classified into lytic and lysogenic types based on their life cycles. Lytic phages, with their specific host range, mitigate antibiotic-related effects on the gut microbiota. Furthermore, their inability to infect eukaryotic cells underscores their clinical utility (11).
Given the imperative to address antibiotic resistance in P. aeruginosa infections and the debate surrounding lytic phage therapy for nosocomial infections in burn patients, our study aimed to investigate the synergistic impact of lytic phages and topical antibiotics in treating burn wounds infected with Pseudomonas aeruginosa. We concurrently administered mupirocin and Abukhalsa burn ointments, acknowledging the contentious choice between combination therapy and monotherapy for managing Pseudomonas infections, and the potential benefits of combination therapy for P. aeruginosa (6, 7).
Bacterial Strains and Bacteriophages Enrichment
This study was conducted in Iran and it focused on evaluating the stability of three phages (see Table1), vB_PA6_GUMS (referred to as PA6), vB_PA32_GUMS (referred to as PA32), and vB_PA45_GUMS (referred to as PA45), within two conventional burn wound care products. All three phages were isolated and characterized for their effectiveness against Pseudomonas aeruginosa (5). Three different Pseudomonas aeruginosa strains were isolated from burn wounds in patients admitted to the Besaat Hospital in Hamadan. These clinical isolates, represented 3 different clones, as determined with pulsed-field gel electrophoresis (PFGE). These bacteria as hosts were stored in 15% glycerol at -80°C. The strains were cultivated in EMB (Eosin Methylene Blue) agar to control for contamination. Subsequently, isolated strains were cultured in LB (Luria Bertani) broth to prepare strains for the experiments. All three bacteriophages were propagated and enriched in LB broth using the agar overlay method (12) and subsequently phage concentrations (approximately 109-1010 pfu/mL) were determined. A summary of the characteristics of the bacteriophages is shown in Table 1.
Burn Wound Care Products and Their Active Ingredients
Two burn ointments were used in this study: (1) Mupirocin (manufactured by Sobhan Daru in Rasht, Iran), wherein each gram comprised 20 mg of mupirocin within a neutral water-miscible ointment base using polyethylene glycol (PEG) 400 and PEG 3350, and (2) Abukhalsa (produced by Darudarman Salafchegan in Tehran, Iran), containing extract from Arnebia Euchroma (AE), sesame oil, and bee wax.
Table 1. The characteristics of three bacteriophages
| Phage Name | Phage vB_PA45_GUMS | Phage vB_PA32_GUMS | Phage vB_PA6_GUMS |
| Host species | P. aeruginosa | P. aeruginosa | P. aeruginosa |
| Source of isolation | soil | sewage | soil |
| Place of isolation | Hamadan | Rasht | Hamadan |
| Family/genus of Caudovirales | Myoviridae | Myoviridae | Myoviridae |
| Genome size (kbp) | 94.2 | 280.2 | 66.8 |
| Accession No. | MN563785 | MN563784 | MN563783 |
Two burn ointments were used in this study: (1) Mupirocin (manufactured by Sobhan Daru in Rasht, Iran), wherein each gram comprised 20 mg of mupirocin within a neutral water-miscible ointment base using polyethylene glycol (PEG) 400 and PEG 3350, and (2) Abukhalsa (produced by Darudarman Salafchegan in Tehran, Iran), containing extract from Arnebia Euchroma (AE), sesame oil, and bee wax.
Stability of Lytic Phages
Two ointments were combined with each of three phage suspensions (with an initial concentration of 109-1010 pfu/mL) in a 1:1 weight per volume (w/v) ratio. Then the mixtures were incubated at 37°C for 24 hours and sampling was conducted in time intervals of 2, 4, and 24 hours (12). After this, the phage concentrations were determined using the agar-overlay method (5). A therapeutic titer of 107 pfu/mL was considered effective (12). Each experiment was conducted three times to obtain a reliable average. As a control, before the stability experiments, each phage was checked for its stability in phosphate-buffered saline (PBS) at 37°C for 24 h.
Statistical analysis
The statistical significance of differences between groups was obtained using repeated measures of one-way analysis of variance (ANOVA) followed by Holm-Sidak's multiple comparisons test. Differences with a P-value<0.05 between experimental groups at each point were considered statistically significant.
Throughout this study, all three annotated bacteriophages show concentrations above the effective therapeutic titer. The comparison of products between different phages is provided in the following sections.
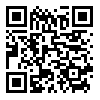
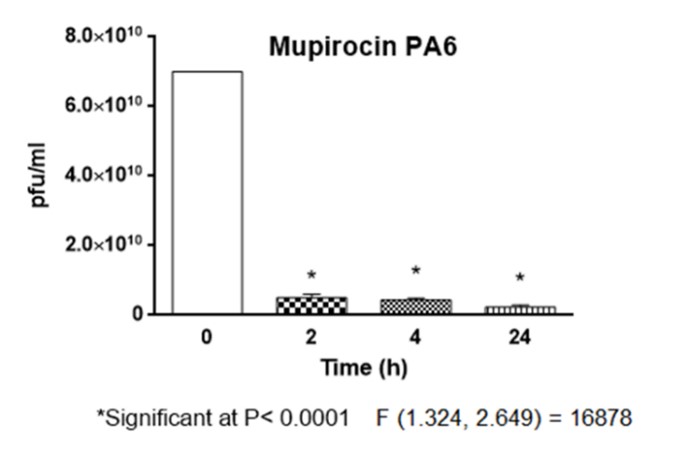
Mupirocin and Phages
Mupirocin influenced the activity of the phages. However, it is important to note that the activity remained above the ETT after 24 hours of incubation. The stability of PA6 shows a significant difference (p < 0.0001) compared to PA45 across all assessed time points (0, 2, 4, 24 h). While PA6 in comparison to PA32 shows no significant difference during intervals 2h, 4h, 24h (P<0.0001). Phage PA45 shows the lowest stability (P<0.0001) against the ointment at all time points (2h, 4h, 24h). PA32 displayed a higher titer (P<0.0001) than PA45 at 2, 4, and 24 hours, besides PA45 had a higher initial concentration than PA32 (P<0.0001) (Fig 1, 2, 3, 4).
Abukhalsa and Phages
Even after 24 hours of phages incubation with Abukhalsa, the phages retained activity levels surpassing the ETT. Across time intervals 2, 4, and 24 h, PA6 consistently demonstrated significantly greater stability compared to PA45 (P<0.0001). Initially, PA6 exhibited notably higher stability than PA32 (P< 0.0001), yet this distinction was not maintained in subsequent assessments (2h, 4h, 24h). Notably, PA45 exhibited the lowest stability (P<0.0001) against the ointment at 2, 4, and 24 hours. Phage PA45 having a significantly higher initial concentration than PA32 (P <0.0001), PA32 displayed a higher titre (P<0.0001) than PA45 after 2, 4, and 24 hours(Figures 5, 6, 7, and 8).
Figure 1. Phage 6 stability in Mupirocin in 2,4,24 h
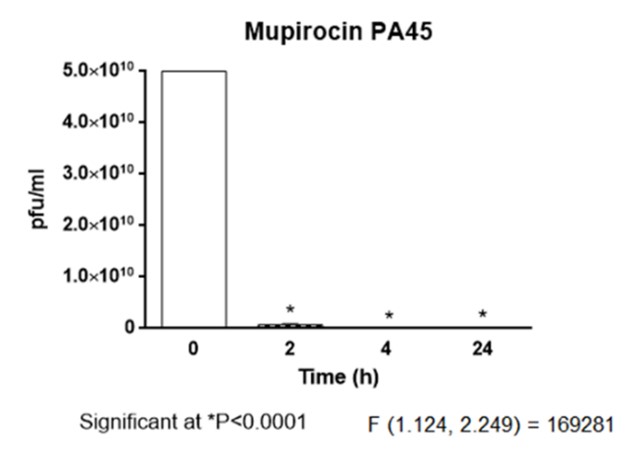
Figure 2. Phage 45 stability in mupirocin in 2,4,24 h
Figure 3. Phage 32 stability in mupirocin in 2,4,24 h
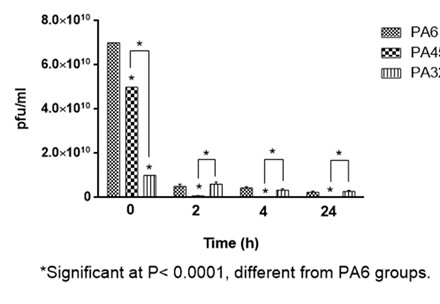
Figure 4. Comparison of three phages in mupirocin in 2,4,24 h
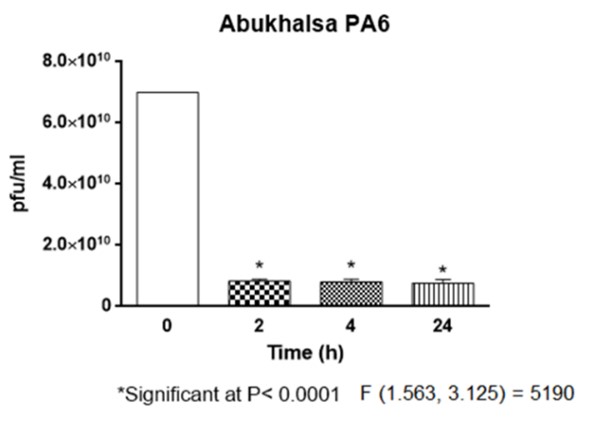
Figure 5. Phage 6 stability in Abukhalsa in 2,4,24 h
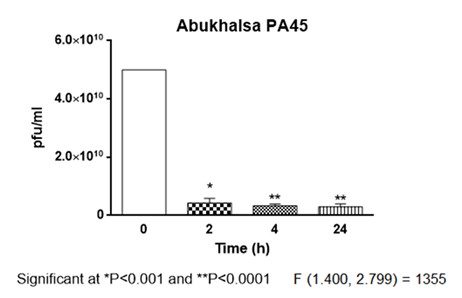
Figure 6. Phage 45 stability in Abukhalsa in 2.4.24 h
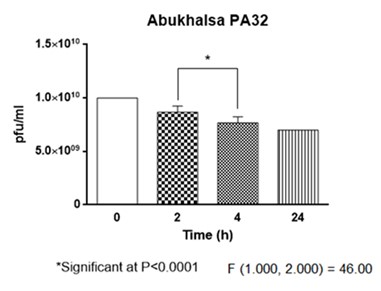
Figure 7. Phage 32 stability in Abukhalsa in2,4,24 h
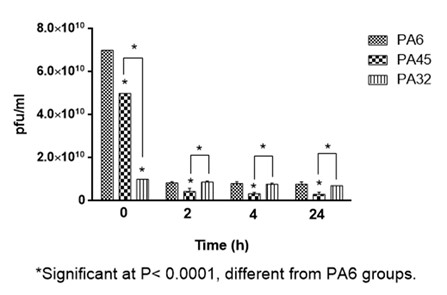
Figure 8. Comparison of three phages in Abukhalsa in 2,4,24 h
The main objective of this study was to evaluate the stability of characterized phages when exposed to two commonly used topical burn ointments for managing burn wounds. Our results indicated that despite the influence of mupirocin on phage activities, their effectiveness remained above the ETT, which is considered above 107 pfu/mL, even after a 24-hour incubation. PA6 and PA32 (as a jumbo phage) that belong to Myoviridae were more stable than PA45(belongs to the Myoviridae family too) in abukhalsa and mupirocin. The increasing interest in the therapeutic use of phages is a consequence of concerns related to bacterial resistance to antibiotics, emphasizing the need for effective alternatives (13).
Nobel Prize laureate Alexander Fleming, who discovered penicillin in 1928, highlighted the risks associated with antibiotic misuse and overuse, emphasizing the potential development of bacterial resistance (14). P. aeruginosa, shows a wide range of inherent resistance to different antibiotic groups, resulting in increased mortality and morbidity rates (15). Multi-drug resistant (MDR) P. aeruginosa, is commonly found in burn patients and causes burn wound infection, leading to elevated sepsis and mortality rates in burnt patients (7). As a result, personalized phage therapy provides an opportunity to counteract bacterial infections, particularly against MDR strains. However, various factors must be considered due to their potential impact on phage stability when used as Active Pharmaceutical Ingredients (APIs). Physicochemical attributes, including the protein structure of bacteriophages, may undergo changes leading to instability in solutions. Environmental factors such as temperature and pH significantly influence phage stability. Additionally, the route of administration and formulation composition further impact phage product activity and availability (16). Each chosen topical burn wound care product for the phage cocktail mixture possesses distinct characteristics like pH values, active ingredients, and ingredient composition that can affect phage stability. Mupirocin is an antibacterial ointment that is active against gram-positive cocci and it is not effective for gram-negative bacilli because it cannot penetrate their cell wall. We assume that a combination of burnt ointments with Pseudomonas aeruginosa-specific phages for topical use may improve the efficacy of infection control (17-21). Abukhalsa with Arnebia euchroma is the other ointment that in some studies shows burn wound healing and decreased infection in burn wounds (22-23), can be also a convenient combination with phages.
Our study found that the activity of all three tested phages (PA6, PA32, PA45) remained above the ETT after 24 hours of incubation within both topical burn wound care products (Mupirocin and Abukhalsa). The experiment involved a combination of the topical burn wound care products and phage suspensions (phage initial concentration approximately 1010pfu/mL) at a 1:1 ratio, followed by phage titer assessment by agar overlay method after 2, 4, and 24 hours of incubation. In a prior study, Aghaee et al. investigated the stability of the same three phages in two distinct topical care products (Nitrofurazone and Silver sulfadiazine). Using the same method, they observed a substantial decline in phage titer below the ETT after 2 hours of incubation (5). This is the reason why we decided to evaluate these phages in other conventional burn ointments such as mupiricin and Abukhalsa.
In another study by Merabishvili et al., the stability of two specific phages against P. aeruginosa was assessed in combination with 13 different topical wound care products, including mupirocin. One of the phages that belong to Myoviridae exhibited notable resilience, maintaining activity above ETT values in 8 mixtures (including mupirocin) after 24 hours. Additionally, the other phage belonging to Podoviridae retained a titer higher than ETT in 5 mixtures after 24 hours (12).
The results of our study include successfully introducing six novel combinations of phages against P. aeruginosa and topical burn wound care products, unexplored before this research. While we examined two routine topical burn wound care products in combination with three major phages against P. aeruginosa, opportunities for exploring additional key agent combinations remain. A combination of two antimicrobial agents can make drug-resistant bacteria decrease in number due to a fitness trade-off (24-28). A fitness trade-off happens when a bacteria faces two external stressors such as the combination of an antibiotic and a phage, in this situation, the bacteria may become resistant against one of these agents but also decrease in virulence factors expression and finally, pathogenesis may decrease (29-31) so using two antimicrobial agents consist of phage and antibiotic in treating burn wound infections with both gram-negative and positive bacteria that are highly resistance to antibiotics can be a wise solution and as a consequence burn wound healing will happen. Furthermore, the short-term nature of this study underscores the need for continued investigation along this trajectory with more combination assessments. This approach aims to identify effective and stable mixtures to address the challenge of antibiotic resistance in burn wound infections.
Our study revealed that three characterized phages such as PA32, PA6, and PA45 were stable for 24 hours when combined with mupirocin and abukhalsa burn ointments. It is also revealed that all three phages maintained their efficacy above the ETT after 1 whole day. It seems PA6 and PA32 (as a jumbo phage) were more stable than PA45 in both tested ointments. The combination of phages and topical burn ointments can improve bacterial infection (caused by both gram-negative and gram-positive bacteria) control in burnt patients, as a consequence examining the stability of the phages is the first step of this theory.
Not applicable.
Ethical Considerations
Ethical Considerations: This study was approved by the Ethics commitment of Mazandaran University of Medical Sciences (Ethical Code: IR.MAZUMS.3.REC.1401.14593).
Authors’ Contribution
Bahareh l.Aghaee designed the project. B.L.A, Omid Mohammad Rezakhani, Erfan Darban Razavi, and Samaneh Farrokhfar did the experiments. Davood Farzin analyzed the results by prism. B.L.A and Alireza Vahdatinia, Parnian Azad Tarighat, S.F, O.M.R and E.D.R wrote the paper together.
This work was supported by Mazandaran University of Medical Sciences, Ramsar Campus.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Received: 2023/12/2 | Accepted: 2024/01/29 | ePublished: 2024/03/18
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |