BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-1016-en.html
2- Department of Pathobiology, Faculty of Veterinary Medicine, University of Shahrekord, Shahrekord, Iran
.
Nosocomial infections cause significant morbidity and mortality worldwide, and the pathogenic organisms that are responsible for such infections may resist antimicrobial agents. Therefore, understanding the activity of commercial disinfectants against environmental and pathogenic bacteria is very important (1) and the need for improved disinfection methods in therapeutic settings is abundantly felt (2). Pseudomonas aeruginosa is an important bacterium responsible for nosocomial infections (3) that may resistant to antibiotics (4). Therefore, it causes multidrug- resistance infections (5). Pseudomonas aeruginosa has a great importance due to its pathogenicity and adaptation to different environmental conditions (6). In addition, it is known to be an important human pathogen that can lead to nosocomial infections, especially in the intensive care unit, immune system disorder, wound infection, skin burn, eye infection, bacteremia, etc (7, 8). Which is a contaminant of medical instruments and causes of cross-infection in hospitals (9). Disinfection methods in hospitals are the main type of intervention against pathogenic microorganisms (10). Based on information reported by the European Center for Disease Prevention and Control (ECDC), About 33,000 people in Europe die each year from infections caused by multidrug-resistant bacteria (11). Eighty- eight thousand deaths from nosocomial infections have been reported in Iran in 1995 (12). In recent years, numerous studies have been conducted in different countries to evaluate the effect of disinfectants and antiseptics against bacterial agents (13). Until now various disinfectants and compositions have been developed by different companies, each has its own disadvantages and advantages. Since manufacturers often exaggerate their product descriptions, it is sometimes difficult to choose a suitable disinfectant. Incorrect use of disinfectants also exposes the bacteria to non-lethal concentrations of these solutions and can subsequently help develop resistance. Therefore, it is necessary to verify the accuracy of the dilution protocols provided by the manufacturing companies before applying their products (13, 14).
Given the aforementioned and the importance of Pseudomonas aeruginosa in the incidence and complication of nosocomial infections and its intrinsic resistance to antibiotics, the use of appropriate methods to control it is very important. Therefore, in the present study, the effect of four disinfectants: Hydrocare, Benzalkonium Chloride, Vico sience and Cetrimide- C,with the dilutions recommended by the manufacturer in inhibiting the growth of Pseudomonas aeruginosa isolates obtained from human infections at different time intervals was investigated.
Sample Collection
For the present study, in May 2019, seven strains were collected from the laboratory of Alzahra Hospital in Isfahan and four isolates along with a standard strain were obtained from Microbial Bank Collection of Faculty of Veterinary Medicine, Shahrekord University.
Verification of Bacterial Samples
Bacterial samples were cultured on MacConkey agar medium and incubated at 37 ° C for 24-48 h. To purify and isolate the proliferating bacteria, one to two similar colonies were cultured on sterile blood agar medium and incubated at 37 ° C for 24–48 h to achieve single and pure colonies.
To confirm the bacterial growth, the colonies were first morphologically and biochemically tested and then cultured in TSB medium and incubated at 37 ° C for 24 hours. After the incubation, the bacteria grown in TSB were re- cultured in blood agar medium. Smears were prepared from the colonies and catalase and oxidase tests were performed (15). Then a single colony was picked out and was cultured on MacConkey agar medium to grow lactose-negative colonies. The bacteria were then cultured on Cetrimide agar medium and the production of brown and green pigments was investigated (16). The colonies were then cultured in TSI medium to evaluate the bacterial ability to consume glucose, lactose, sucrose and also hydrogen sulfide gas production, alkaline reaction and not fermenting sugar (16). At a later stage, colonies were cultured in SIM medium to test for SH2 and indole production, and bacterial motility. Subsequently, colonies were cultured on Lithmus Milk medium to observe the color change and fragmented clots (15).
Evaluation of the Effect of Disinfectants on Pseudomonas aeruginosa Strains
Hydrocare is a very powerful detergent and disinfectant that is used to prevent infectious diseases caused by drinking water (17). According to the guidelines provided by Dominteb Company, Iran, a dilution of 4:100 Hydrocare disinfectants will be effective.
At first the stoke solution (4:100) of Hydrocare was prepared by adding 400 μL of Hydrocare to 9.6 ml of sterile distilled water. Then 1 ml of the stock solution was added to 9 mL of Yeas Extract Broth medium.
Vico sience is a rapid eliminator of a wide range of pathogens (18). According to the guidelines provided by Sciene Laboratories (LS), a dilution of 1:100 Vico sience disinfectants will be effective. To prepare a stock solution (1: 10) of Vico sience, 1 g of disinfectant was dissolved 9 ml of sterile distilled water. Then 1 ml of stock was dissolved in 9 ml of Yeas Extract Broth medium.
Benzalkonium Chloride is a broad spectrum biocide (19) that has various applications in disinfection industry (20, 21), medicine (22) and home use (23). According to the guidelines provided by Benzalkonium Chloride (license number: D.T-140-93, Veterinary Organization), a dilution of 1:200 Benzalkonium Chloride disinfectants will be effective.
To prepare stock solution (1:200) of Benzalkonium Chloride 1 mL of disinfectant was dissolved in in 19 mL of sterile distilled water. Then, 1 mL of stock solution was added in 9 ml of Yeas Extract Broth medium.
Cetrimide-C or Savlon is a widely used disinfectant that is applied for disinfection and bandage, rinsing and disinfecting hospital equipment and the operating room, etc. It is a strong bactericidal, safe and free of toxic effects (24). According to the guidelines provided by Cetrimide-C (license number: SH- 67- 013, Iran Daru Laboratory), a dilution of 1:200 Cetrimide-C disinfectants will be effective. For the preparation of Stoke solution (1:200) Cetrimide-C 1 mL of the disinfectant was dissolved in 19 ml of sterile distilled water. Then, 1 mL of obtained stock solution was added in 9 mL of Yeas Extract Broth medium.
To investigate the effect of disinfectants on Pseudomonas aeruginosa isolates, 2–3 colonies were picked up from the purified culture of each strain and cultured in tubes containing TSB medium. After the incubation at 37 ° C for 24 hours, the turbidity of the tubes was compared with 0.5 McFarland standard turbidity
(2.5 × 108 CFU / mL). Whereas the turbidity of the tubes containing the bacterial strain was higher than the 0.5 McFarland standard, the BHI environment was added and if the absorbance of the bacterial strain was lower than the standard, the bacterial colony was added to achieve a concentration equal to the 0.5-McFarland standard.
Subsequently, 100 µL of the obtained 0.5-McFarland medium was added to 9.9 mL of TSB medium to give the concentration of strains at 2.5 × 106 CFU / mL.
Then 100 microliter of bacterial strain at a concentration of 2.5 × 106 CFU / mL was added to tubes containing 9.9 mL of Yeas Extract Broth mixed with a disinfectant stock and it was completely mixed. At the times 5, 10, and 15 minutes after mixing the disinfectant dilution with the bacterial strain, 1 mL of the mixture of disinfectant and bacteria was added to 3 mL of BHI Broth and after a complete mixing, it was incubated at 37 ° C for 4 days. After this period of time, 50 μL of the mixture of disinfectant and bacteria was seeded on a Nutrient agar medium and then it was incubated at 37 ° C for 24 h. At the end, the growth or non-growth of bacterial colonies in was studied.
Confirmation of Pseudomonas aeruginosa Isolates
The results of biochemical tests performed for purified colonies has been shown in Figure 1.
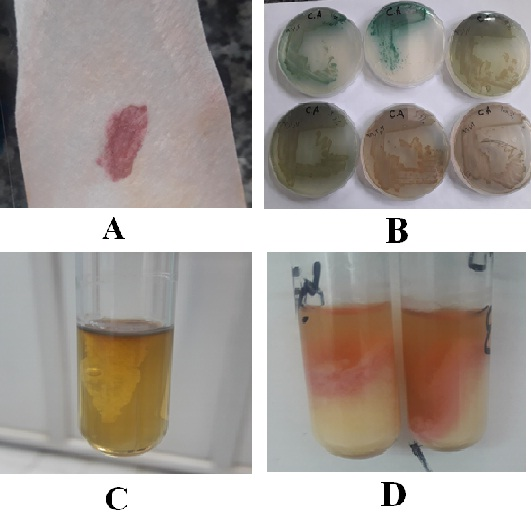
Figure 1. Confirmation of Pseudomonas aeruginosa isolates
A: Oxidase test, the colony is dark purple and confirms Pseudomonas aeruginosa.
B: Cetrimide agar test, produces brown and green pigments and confirms Pseudomonas aeruginosa.
C: SIM test, inverted cedar view which is a sign of movement and confirmation of Pseudomonas aeruginosa.
D: Lithmus Milk test, the pink environment is white with patches and confirms Pseudomonas aeruginosa.
Investigating the Effect of Each of the Tested Disinfectants on Pseudomonas aeruginosa Isolates.
The results of this study to investigate the antimicrobial effect of four disinfectants, Hydrocare, Benzalkonium Chloride, Cetrimide-C and Vico science in eliminating Pseudomonas aeruginosa isolated from human infections in hospitals, in terms of whether the recommended concentration is in the instructions. Disinfectants affect the removal of Pseudomonas aeruginosa species in hospital centers, to what extent is the manufacturer's instructions correct and to what extent has it simply deviated from the introduction of products?
According to Table 1, in 5, 10 and 15 minutes no bacterial growth was observed in any of the isolates. In other words, the disinfectant Hydrocare kills the bacteria completely and has a 100% effect on the bacterium Pseudomonas aeruginosa.
According to Table 2, in 5, 10 and 15 minutes no bacterial growth was observed in any of the isolates. In other words, the disinfectant Benzalkonium Chloride kills the bacteria completely and has a 100% effect on the bacterium Pseudomonas aeruginosa.
Table 1. The effect of the disinfectant Hydrocare on Pseudomonas aeruginosa isolates
| 15 minutes | 10 minutes | 5 minutes | strains name |
|---|---|---|---|
| Non-growth | Non-growth | Non-growth | Standard |
| Non-growth | Non-growth | Non-growth | Strains1 |
| Non-growth | Non-growth | Non-growth | Strains2 |
| Non-growth | Non-growth | Non-growth | Strains3 |
| Non-growth | Non-growth | Non-growth | Strains4 |
| Non-growth | Non-growth | Non-growth | Strains5 |
| Non-growth | Non-growth | Non-growth | Strains6 |
| Non-growth | Non-growth | Non-growth | Strains7 |
| Non-growth | Non-growth | Non-growth | Strains8 |
| Non-growth | Non-growth | Non-growth | Strains9 |
| Non-growth | Non-growth | Non-growth | Strains10 |
| Non-growth | Non-growth | Non-growth | Strains11 |
| 100% Non-growth | 100% Non-growth | 100% Non-growth | Total |
Table 2. The effect of the disinfectant Benzalkonium Chloride on Pseudomonas aeruginosa isolates
| 15 minutes | 10 minutes | 5 minutes | strains name |
| Non-growth | Non-growth | Non-growth | Standard |
| Non-growth | Non-growth | Non-growth | Strains1 |
| Non-growth | Non-growth | Non-growth | Strains2 |
| Non-growth | Non-growth | Non-growth | Strains3 |
| Non-growth | Non-growth | Non-growth | Strains4 |
| Non-growth | Non-growth | Non-growth | Strains5 |
| Non-growth | Non-growth | Non-growth | Strains6 |
| Non-growth | Non-growth | Non-growth | Strains7 |
| Non-growth | Non-growth | Non-growth | Strains8 |
| Non-growth | Non-growth | Non-growth | Strains9 |
| Non-growth | Non-growth | Non-growth | Strains10 |
| Non-growth | Non-growth | Non-growth | Strains11 |
| 100% Non-growth | 100% Non-growth | 100% Non-growth | Total |
According to Table 3, Cetrimide-C disinfectant has seen approximately 3 growths from 12 isolates in 5 minutes and 100% bacterial growth in the other 9 strains. In the 10 minutes that most strains came in contact with disinfectants, about 4 strains of bacterial growth were not observed, and in the other 8 strains, 100 bacterial growths were observed. Within 15 minutes, when the strains were much higher in contact with disinfectants, no bacterial growth was observed in 4 strains and 100 bacterial growths were observed in the other 9 strains. According to the Cetrimide-C disinfectant, of the 12 isolates tested for Pseudomonas, 2 were effective: 1 and 10 isolates and it kills bacteria and prevents them from growing 10%, in Separation No. 9, contact with less disinfectant affects the bacteria, which is observed in 5 and 10 minutes 20% without growth and in 15 minutes it has been ineffective. Separation of No. 2 at low contact times, in 5 minutes, was ineffective and in 10 minutes, it had a 10% effect on killing bacteria in contact with disinfectants for more than 15 minutes, the effect is greater and the bacteria does not grow 20%. In general, the antiseptic effect of Cetrimide-C on 12 strands of Pseudomonas aeruginosa in 5 minutes 20%, 10 minutes 25% and 15 minutes 30% prevents the growth of bacteria and the bacterium has sometimes been able to grow despite the presence of the Cetrimide-C disinfectant.
Table 3. The effect of the disinfectant Cetrimide-C on Pseudomonas aeruginosa isolates
| 15 minutes | 10 minutes | 5 minutes | strains name |
| 100% growth | 100% growth | 100% growth | Standard |
| 90% growth | 90% growth | 90% growth | Strains1 |
| 80% growth | 90% growth | 100% growth | Strains2 |
| 100% growth | 100% growth | 100% growth | Strains3 |
| 100% growth | 100% growth | 100% growth | Strains4 |
| 100% growth | 100% growth | 100% growth | Strains5 |
| 100% growth | 100% growth | 100% growth | Strains6 |
| 100% growth | 100% growth | 100% growth | Strains7 |
| 100% growth | 100% growth | 100% growth | Strains8 |
| 100% growth | 90% growth | 90% growth | Strains9 |
| 90% growth | 90% growth | 80% growth | Strains10 |
| 100% growth | 100% growth | 100% growth | Strains11 |
| 30% Non-growth | 25% Non-growth | 20% Non-growth | Total |
According to Table 4, the Vico science disinfectant has not been effective in just 5 minutes at 80%, and only in isolating No. 11, 100% growth of bacteria was observed. Colon growth was not observed at any time of 10 min or 15 min and 100% disinfectant has not caused the growth of bacteria. In other words, the Vico science disinfectant has been quite effective in 11 Shush from the beginning and in the other Strains, it was not only effective in the first 5 minutes and with more contact, the disinfectant with the bacteria in 10 minutes and 15 minutes has completely destroyed the bacteria.
Table 4. The effect of the disinfectant Vico science on Pseudomonas aeruginosa isolates
| 15 minutes | 10 minutes | 5 minutes | strains name |
| Non-growth | Non-growth | Non-growth | Standard |
| Non-growth | Non-growth | Non-growth | Strains1 |
| Non-growth | Non-growth | Non-growth | Strains2 |
| Non-growth | Non-growth | Non-growth | Strains3 |
| Non-growth | Non-growth | Non-growth | Strains4 |
| Non-growth | Non-growth | Non-growth | Strains5 |
| Non-growth | Non-growth | Non-growth | Strains6 |
| Non-growth | Non-growth | Non-growth | Strains7 |
| Non-growth | Non-growth | Non-growth | Strains8 |
| Non-growth | Non-growth | Non-growth | Strains9 |
| Non-growth | Non-growth | Non-growth | Strains10 |
| Non-growth | Non-growth | Growth100% | Strains11 |
| 100% Non-growth | 100% Non-growth | 92% Non-growth | Total |
Confirmation of the Effect of Disinfectants Tested on Pseudomonas aeruginosa Isolates
The results effects of the disinfectants tested on the Pseudomonas aeruginosa isolates can be seen in Figure 2.
Comparing the Effect of Disinfectants with Pseudomonas aeruginosa Isolates
The results of the present study to investigate the antimicrobial effect of four disinfectants of Hydrocare, Benzalkonium Chloride, Cetrimide-C and Vico science against Pseudomonas aeruginosa isolates obtaibed from human infections are summarized table 1. According to the information presented in this table, Hydrocare and Benzalkonium Chloride caused 100% non- growth at all 3 times of 5, 10 and 15 minutes. Vico science resulted in 100%, 100% and 92% at 15, 10 and 5 minutes bacterial non- growth, respectively. Cetrimide-C showed 20%, 25%, and 30% inhabitation of bacterial growth at 5, 10 and 15 minutes, respectively, and using ANOVA statistical test the difference in the antiseptic power of Citrimide-C was statistically significant (P<0.05).
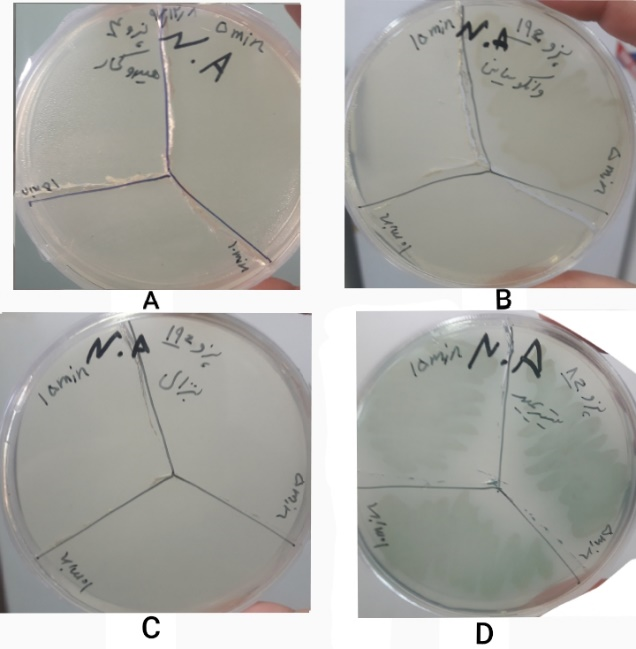
Figure 2. Confirmation of the Effect of Disinfectants on Pseudomonas aeruginosa
A: The effect of the disinfectant Hydrocare on Strains4, at all three times, the bacteria did not fully grow for 5, 10, and 15 minutes.
B: The effect of the disinfectant Vico science on Strains11, (In the form of: 19z sample number in the hospital), the disinfectant did not work for 5 minutes and the bacteria grew Colonial growth was not observed at 10 min and 15 min, and the disinfectant had a 100% effect.
C: The effect of the disinfectant Benzalkonium Chloride on Strains11, at all three times, the bacteria did not fully grow for 5, 10, and 15 minutes.
D: The effect of the disinfectant Cetrimide-C on Strains 8, At all three times, the bacteria were fully formed for 5, 10 and 15 minutes.
Table 5. The effect of the disinfectants on Pseudomonas aeruginosa isolates (12 strains)
| 15 minutes | 10 minutes | 5 minutes | Disinfectant name |
| 100% Non-growth | 100% Non-growth | 100% Non-growth | Hydrocare |
| 100% Non-growth | 100% Non-growth | 100% Non-growth | Benzalkonium chloride |
| 100% Non-growth | 100% Non-growth | 92% Non-growth | Vico sience |
| 30% Non-growth | 25% Non-growth | 20% Non-growth | Cetrimide- C |
In this study, it was very difficult to determine which disinfectant was the most potent; although the results from Cetrimide- C were very poor, the three other disinfectants did not differ significantly. The results showed that Cetrimide- C may not be suitable and useful for control of Pseudomonas aeruginosa in health centers and hospitals and if is used according to the manufacture instructions, it will not only has the ability to inhibit bacterial growth but can also cause irreparable damages.
Along with the present study, other studies have been carried out including:
El-Bana et al. (2019) studied the effect of non-lethal concentrations of Benzalkonium Chloride on the antibiotic resistance, growth pattern and biofilm formation of Pseudomonas aeruginosa isolates and the results indicated that 60% of isolates showed increased biofilm formation and antibiotic resistance (25).
Montagna et al (2019) evaluated the effect of five hospital antibacterial disinfectants (Phenolic compounds, Quaternary Ammonium compounds, Sodium hypochlorite, alcoholic compounds and Hydrogen peroxide) on Pseudomonas aeruginosa, Staphylococcus aureus and Enterococcus. The results showed that Hydrogen peroxide at all concentrations was the only disinfectant that had inhibitory effect against all tested microorganisms (1).
Vijaya et al. (2016) addressed the issue of increasing the drug resistance of Pseudomonas aeruginosa clinical strains against common disinfectants in the laboratory, it has been shown that aerogenous strains increase by 22% multidrug resistance as well as decrease resistance to benzalkonium chloride disinfectant (26). Medical environments, etc., may be infected with microorganisms, which are disinfected with disinfectants such as benzalkonium chloride. Of course, various factors can be involved in the resistance of pathogens to this disinfectant.
Hourai et al. (2004) studied the disinfectant effect of benzalkonium chloride and chlorhexidine on bacterial biofilm formation, the bacterium Pseudomonas aeruginosa is more resistant to the disinfectant benzalkonium chloride. The results of the study by Hourai et al. Did not show much agreement with the present study, because in our study, benzalkonium chloride showed a 100% inhibitory effect against the growth of Pseudomonas aeruginosa bacteria. The reason for this discrepancy may be due to differences in the methods used in the two studies as well as differences in the studies studied (27).
Carson et al. (1972) examined the factors affecting the resistance of Pseudomonas aeruginosa purified from a hospital center to disinfectants, they found that Pseudomonas aeruginosa was inactivated by contact with glutaraldehyde chloride, acetic acid, and a combination of ammonium quaternary, this inactivation depends on factors such as the growth stage at the time of contact with the disinfectant, the nature of the disinfectant, and the incubation temperature. The results of a study by Carson et al. On the effect of ammonium quaternary compound on Pseudomonas aeruginosa were consistent with the results of the present study (28).
Olasehinde et al. (2008) addressed the effect of Savlon, Dettol, la-naphtho disinfectants on Pseudomonas aeruginosa, Salmonella typhoid and Proteus bacteria. In this study, the concentration of disinfectants was increased by 25% and the results showed that all disinfectants had weaker inhibitory inhibition than microorganisms in the early stages, As the concentration increased, the disinfectant effect increased (29). The findings of this study on the weakness of the antimicrobial effect of Saulen are in line with the findings of the present study.
Hassan et al. (2008) examined the effect of a number of common hospital disinfectants against Pseudomonas aeruginosa isolated from patients' infections. The strains studied showed resistance to the three ethanol disinfectants, Jeremy Side-P and Pidon Ayodine with different dilutions in the surface test with different percentages and only Cetrimide-C was able to completely eliminate all strains by consuming 1 to 30 (30). The reason for the discrepancies between the findings of this study and the results of the present study is that the concentration of 1 to 30 Savlon used in the study of Hassan et al. Is much higher than the concentration recommended by the manufacturing plant in the present study.
Gasparini et al. (1995) discussed the effect of Virkon S on Pseudomonas aeruginosa, Escherichia coli, Staphylococcus aureus and Spor bacillus bacteria, and hepatitis B surface antigen, Virkon S was in contact with the mentioned bacteria for 5, 10, 20, 30, 40, 50, 60 minutes and they found that Virkon S was able to destroy the surface antigen of hepatitis B. They also found that Virkon S was suitable for destroying spores. The results of this study showed that Virjon S is a very fast disinfectant. The results of the Gasparini et al. Study of the effect of vacuoussion on Pseudomonas aeruginosa are fully consistent with the results of the present study (31).
The present study is based on a Master's thesis in Bacteriology at Shahrekord University. The authors are grateful to the personnel of the Microbiology Laboratory of the Faculty of Veterinary Medicine, Shahrekord University.
Authors declared no conflict of interests.
Received: 2019/12/23 | Accepted: 2020/05/4 | ePublished: 2020/03/9
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







