BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-939-en.html
2- Department of Gastroenterology, Gastrointestinal and Liver Diseases Research Center (RCGLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
3- Department of Infectious Diseases, Hepatitis Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
4- Department of Emergency Medicine, Besat Hospital, AJA University of Medical Sciences, Tehran, Iran
5- Infectious Diseases and Tropical Medicine Research Center (IDTMRC), AJA University of Medical Sciences, Tehran, Iran ,
.
Hospital- acquired infections (HAIs) are infectious diseases an individual experiences 48 hours post- hospitalization, 3 days following hospital discharge, or 30 days after a surgery. Therefore, the patients has not have the infection before hospitalization nor has the patient been in the latent period of the disease (1, 2). HAIs often develop through contaminated medical equipment at the surgical site or through antibiotic-resistant pathogens. These infections are not limited to the patient, but also affect hospital specialists and staff. According to the recent reports, only 20% of nosocomial infections are preventable (3). The World Health Organization (WHO) has identified nosocomial infections as a major cause of disability and death among patients (7). The actual rate of HAIs varies from 5-10% among modern health centers in developed countries and up to 25% in developing countries, which is about 2-20 times higher among developing countries compared to developed countries. This rate has been reported to be 1.9 to 25 percent in Iran (9) which is mostly due to surgery site infections (58.2%), pneumonia (26.4%) and urinary tract infections (8.8%) (10), respectively.
In this review, we will discuss the most important pathogens responsible for nosocomial infections as well as multidrug-resistant (MDR) pathogens as a major threat around the world.
PubM, Medline, Cochran library, WHO, Iranmedex and PsycINFO databases were searched for articles related to different aspects of nosocomial infections and bacterial resistance, published during 1980 and 2018. An evaluation regarding the association between nosocomial infections and bacterial resistance with the use of antibiotics were carried out in March 2017.
Research on nosocomial infections was conducted in two steps. The first step was to examine the aspects and issues related to nosocomial infection, and the second step was to investigate the relationship between bacterial resistance and challenges. To gather information on nosocomial infections and bacterial resistance, the following keywords were searched: resistant bacteria, nosocomial infections, antibiotics, multidrug-resistant drugs, Healthcare, Pathogens.
Out of a total of 182 articles found following the key word search, 28 articles were relevant, in terms of subject and content, and were therefore included in this article.
Important causes of nosocomial infections
About 90% of nosocomial infections are caused by bacteria. Bacteria that commonly cause nosocomial infections include Staphylococcus spp. especially S. aureus, Streptococcus spp., Bacillus cereus, Acinetobacter spp., enterococcus spp., Pseudomiononas aeroginosa. Escherichia coli, Proteus mirabilis, Salmonella spp., Serratia marcescens and Klebsiella pneumonia, among which E. coli, S. aureus, enterococcus spp. and P. aeruginosa are the most common causes of nosocomial infections (7, 8, 13).
In hematologic infections (BSI), coagulase negative Staphylococci are common and are isolated almost twice as much as S. aureus among patients with BSI (13, 17).
Enterococcus spp. have been repeatedly isolated from surgical site and bloodstream infections, but is rarely found in the respiratory tract. P. aeruginosa has been isolated from one-tenth of all infections and is found equally in all areas prone to nosocomial infections with the exception of blood stream (13).
Viruses cause only 5% of nosocomial infections and are more common among infants and children. There are possibilities of transmitting nosocomial infections caused by viruses, including hepatitis B and C viruses (via dialysis, injection, endoscopy), respiratory syncytial virus (RSV), rotavirus, and enterovirus (through hand-to-mouth and mouth- to- mouth contact) in the hospital (19, 20).
Some parasites are easily transmitted between children and adults. Many fungi and parasites are opportunistic organisms that cause infections during long-term treatment with antibiotics. Environmental contamination caused by organisms that spread through the air, such as Aspergillus spp., is a concern during hospital construction (13, 21).
The importance and impact of using antibiotics in nosocomial infections
In developing countries, drugs such as antibiotics are easily available in pharmacies (12) and the overuse of a wide range of antibiotics in the hospital environment has led to the emergence of MDR microorganisms which cause fatal nosocomial infections and are difficult to treat (13, 22).
The most important MDR bacteria causing nosocomial infections include E. faecium, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter species, which are classified as ESKAPE.
In addition, in 2017, WHO published a list of the most important bacterial species and the antibiotics against which these bacteria are resistant (Table 1). This group of pathogens is responsible for most MDR nosocomial infections (12, 25).

Figure 1. The most common site of nosocomial infections
Table 1. The most threatening bacterial species/families of bacteria and the antibiotics against which the bacteria are resistant (21)
| Antibiotics | Bacteria |
|---|---|
| Carbapenem | A. baumannii |
| Carbapenem | P. aeruginosa |
| Carbapenem | Enterobacter Species |
| Vancomycin | E. faecium |
| Methicillin-Vancomycin | S. aureus |
| Clarithromycin | H. pylori |
| Fluoroquinolones | Campylobacter Species |
| Fluoroquinolones | Salmonella spp. |
| -Fluoroquinolones Cephalosporins | Neisseria gonorrhoeae |
| Penicillin | Streptococcus pneumonia |
| Ampicillin | Hemophilus Influenza |
| Fluoroquinolones | Shigella Spp. |
MDR bacteria that cause nosocomial infections are able to spread and multiply rapidly not only in health care centers but around the world (12). In Europe, over four years (2014-2011), a significant increase in the mean rate of E. coli resistance to third-generation cephalosporins (from 9.6 to 12%), K. pneumonia to carbapenems (from 6.6 to 7.3) P. aeruginosa to carbapenems (from 16.8 to 18.3%) and Enterococci resistance to vancomycin (from 6.2 to 7.9) was observed. In Iran, a study found that 73.8% of the E. coli isolates were resistant to nalidixic acid, 54.3% to Sulfamethoxazol and 54.3% to Liprofloxacin (46).
In order to maintain the efficiency of antibiotics, many hospitals reserve certain antibiotics such as vancomycin and imipenem, only for cases in which other antibiotics have proven ineffective. The problem with this policy is the delay in the use of effective antibiotics in urgent cases. In addition, the limited use of these antibiotics has led to a decline in motivation and ultimately to defect in pharmaceutical industries due to poor investment returns. In fact, the lack of new antibiotics on the market increases the problem of antibiotic resistance (12).
Since the countdown to the emergence of resistance against the newly made antibiotics starts as soon as they are introduced to the clinical settings, the development of new antibiotics is not the ultimate solution to the antibiotic crisis. It is clear that antibiotic resistance is not a one-dimensional problem, and in addition to the sustainable development of new antibiotics, other strategies, including effective vaccines and faster and more sensitive diagnosis, can reduce the emergence of resistance to the new antibiotics (12, 23).
Methicillin-resistant Staphylococcus aureus (MRSA)
S. aureus is a gram-positive bacterial strain and one of the most dangerous bacterial pathogens that can cause nosocomial infections worldwide.
According to the latest research, most S. aureus isolates have been resistant to the antibiotics Cefoxitin, Azithromycin, Cefotaxime, Tetracycline, Gentamycin, Chloramphenicol and Ciprofloxacin (Figure 2).

Figure 2. Antibiotic resistance pattern of S. aureus isolates against different antibiotics (26)
Azi: Azithromycin, Tet: Tetracycline, Gen: Gentamicin, Cip: Ciprofloxacin, Cef: Cefotaxime, Chlo: Chloramphenicol, Cefo:Cefoxitin, and Oxa: Oxacillin
Since resistance to anti-MSRA antibiotics occurs through bacterial mutations, resistance to linezolide and glycoprotein antibiotics has recently become a major concern (27, 31).
Vancomycin resistant Enterococci (VRE)
Enterococci are the second leading cause of nosocomial infections worldwide and the leading cause of infections in the United States (20-30% of infections).
According to a report by the World Health Network, these pathogens cause about 12 percent of all nosocomial infections and kill 1,300 people a year (36). About 35.5% of enterococci are resistant to vancomycin which is created by the synthesis of a modified cell wall precursor that does not bind to glycopyptide antibiotics. This process occurs by the acquisition of a plasmid-dependent gene cluster (mostly vanAog and vanB genes) (36, 37). These may be transferred from enterococci to MSRA and, therefore, further complicate the treatment process of nosocomial infections.
Enterococcus species are less likely to cause nosocomial infections compared to S. aureus. Two of the most important species of Enterococci include E. faecalis and E. faecium. VRE nosocomial infections are mostly caused by E. faecium. Resistant isolates of this species usually possess the resistance genes VanA, VanB, VanD, VanN and VanM, and epidemiological studies have shown that VanA and VanB are the most common types, abundance of which is increasing (Figure 4 and Table 2) (35, 37, 39).
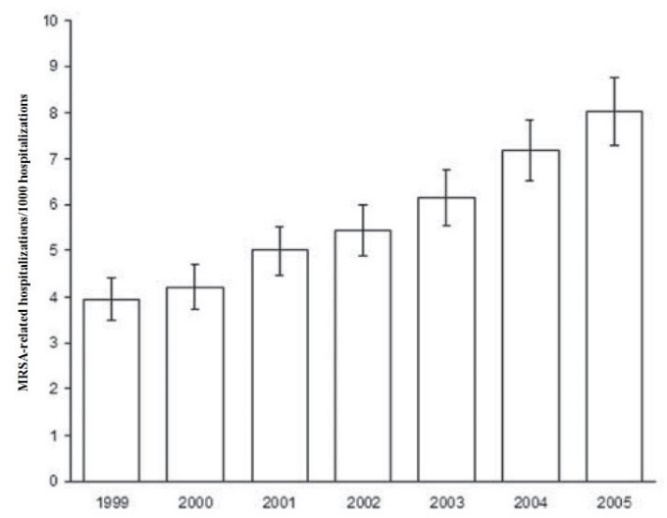
Figure 3. Rate of hospitalizations related to MRSA infections between 1999 and 2005 (27).
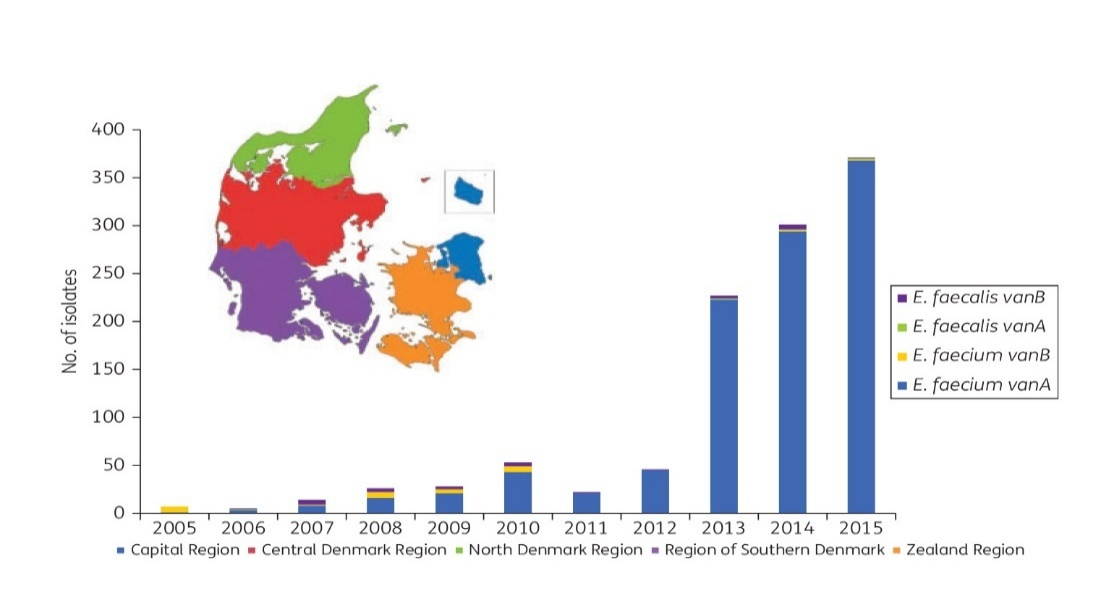
Figure 4. The frequency of the two main VRE species (including E. faecalis and E. faecium) isolated from clinical specimens between 2005 and 2015 (37)
Multidrug-Resistant Klebsiella pneumoniae (MDR-KP)
Klebsiella pneumoniae is a gram-negative bacillus found in a variety of environments, including the human body, gastrointestinal tract, skin, and nasopharynx. Due to the specific pathogenic properties of K. pneumoniae, including capsule production, antibiotic resistance, and biofilm formation, the nosocomial infections caused by this species are typically chronic and difficult to treat.
In recent years, MDR-KP strains have emerged due to the overuse of various antibiotics to treat nosocomial infections caused by this pathogen. MDR-KP is resistant to a wide range of antibiotics, including ampicillin and cephalosporins, which have previously been shown to be effective in treating K. pneumoniae isolates. The global prevalence of MDR-KP strains has become a global threat and concern due to its prevalence in hospitals and community (41, 51). Unfortunately, the optimal options for treating MDR-KP infection have not yet been identified (44, 45). Currently, a combination of clostin, phosphomycin, tigcycline, and aminoglycosides, although associated with adverse outcomes, is widely used. Recently, WHO has warned that if appropriate solutions are not adopted to prevent the development of MDR-KP, current antibiotics would completely lose their effect fail to treat these infections (55, 56).
Multidrug-resistant Acinetobacter baumannii (MR-AB)
A. baumannii, a gram-negative aerobic bacterium, is another important pathogen causing nosocomial infection. ICU is known as the main center for infections caused by A. baumannii, however, several studies have shown that it is possible for this specie to spread it to other areas in the hospital. This pathogen is responsible for about 2-10% of infections caused by all gram-negative bacteria in European and American countries (59-57).
The constant presence of A. baumannii in different parts of the hospital has caused this pathogen to be in constant contact with antibiotics. Such environmental conditions has imposed pressure on the selection and emergence of colonies with antibiotic resistance characteristics. Over time, the emergence if strains that are resistant to 3 or more antibiotic classes, including carbapenems which once were the treatment option of A. baumanii isolates, has increased (61). Due to the increasing resistance of this pathogen against carbapenems and clostin, as the last lines of treatment, therapeutic options are very limited and in some cases do not exist (61, 65).
Multidrug-resistant Pseudomonas aeruginosa (MDRPA)
P. aeruginosa is another gram-negative and aerobic bacterium which is known to be one of the leading causes of nosocomial infections, accounting for 10% of all nosocomial infections (63, 64).
Resistance rates to imipenem, quinolones, and third-generation cephalosporins have increased among P. aeruginosa isolates by 15, 9, and 20 percent, respectively (67).
Of great concern is the results of a recent study showing a significant increase in the rate of MDRPA from 2007 to 2014 (Figure 5).
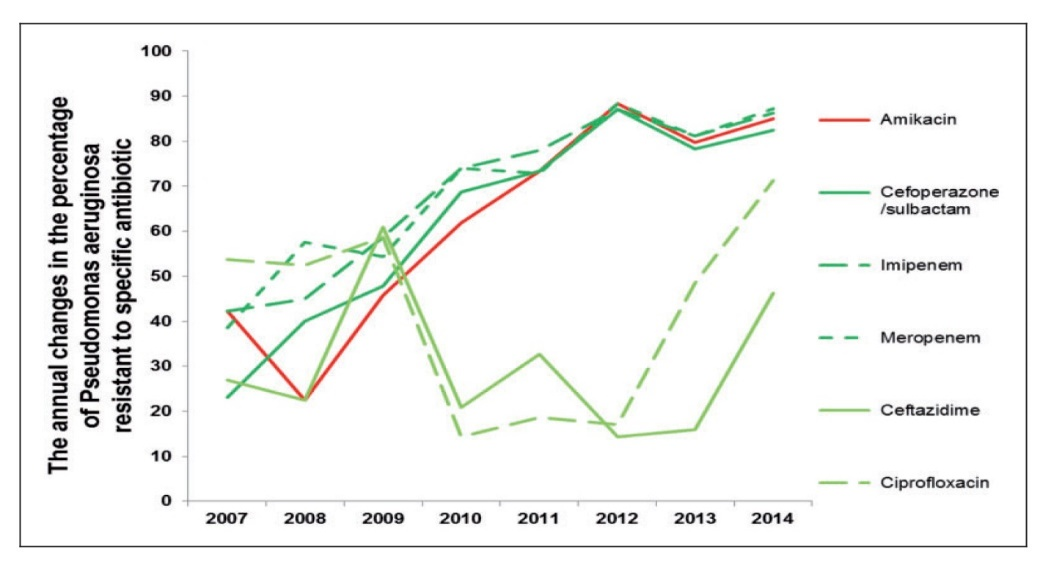
Figure 5. Annual resistance of MDRPA to specific antibiotics from 2007 to 2014 (58).
Studies evaluated in this review reported an important role of antibiotic resistance in imposing therapeutic challenges and mortality among infected patients. Studies have described this factor as a global threat associated with the increase in nosocomial infections among patients. Improper use of a wide range of antibiotics against pathogens responsible for nosocomial infections has led to the emergence of MDR isolates that cause fatal nosocomial infections and are difficult to treat. Therefore, nosocomial infections are still uncontrollable during antibiotic era.
Although the production of new antibiotics are needed to treat nosocomial infections, this alone cannot be a solution to overcome the problem of MDR nosocomial infections. Therefore, some scheduled programs are needed to prevent the improper use of antibiotics and the occurrence of antibiotic resistance in the hospital settings.
The authors thank all those who helped them writing this article.
Authors declared no conflict of interests.
Received: 2019/05/26 | Accepted: 2020/04/14 | ePublished: 2020/05/30
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |