BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-2441-en.html


 , Asmaa Haseeb Hwaid2
, Asmaa Haseeb Hwaid2 

 , Hula Younis Fadhil3
, Hula Younis Fadhil3 

 , Iman M. Aufi1
, Iman M. Aufi1 

 , Ihab R. Aakef1
, Ihab R. Aakef1 

 , Ahmed A. Hussein1
, Ahmed A. Hussein1 

 , Noora A. Abdulhadi1
, Noora A. Abdulhadi1 


2- Department of Biology, College of Education for Pure Sciences, University of Diyala, Diyala, Iraq ,
3- Department of Biology, College of Science, University of Baghdad, Baghdad, Iraq
Crimean-Congo Hemorrhagic fever (CCHF) is a highly consequential zoonotic disease characterized by fatality rate reaching 50% (1, 2). It is a viral disease transmitted through the bites of infected ticks. There are other ways of transmission such as direct contact with blood and tissues from infected individuals and cattle or crushing the infected tick on an open wound. Sometimes sexual intercourse may be considered another way to transmit the virus, as indicated by previous studies (3). The Middle East, Asian countries, Africa and the Balkan countries are endemic centres for ticks that transmit this virus (4).
CCHF is a single-stranded, spherical enveloped RNA virus (5). It is a member of the genus Orthonairovirus that belongs to the family Nairoviridae and the order Bunyavirales (6, 7). The reservoirs and vectors responsible for the persistence of the virus in nature are species of ticks that belong to the genus Hyalomma within the family Ixodidae. The members of this genus are the most important vectors that play major roles in transmitting the virus to humans and various groups of wild and domestic animals (8). The continued emergence of CCHF outbreaks from time to time remains one of the main issues at the level of national and global health security. The steady increase in cases of CCHF infection in recent years has prompted the World Health Organization (WHO) to list it among priority diseases in terms of research and development due to the virus ability to cause devastating epidemics in humans (9). The incidence of CCHF disease in the past decade has increased in the Eastern Mediterranean region. There has been an increase in infection and death rates until the moment of writing the current study due to the continued spread of ticks to transmit the virus, the lack of comprehensive epidemiological surveys and surveillance systems, the failure to understand the epidemiology of the virus, and the risk of increased transmission (10, 11). Iraq like Iran and Turkey, one of the Eastern Mediterranean countries, is an endemic country for CCHF disease. According to the studies, livestock and sheep that are widely raised in Iraq are commonly infected with different types of ticks, especially species of the genus Hyalomma, which are the main vectors of CCHF (12, 13, 4). In animals, the infection progresses without symptoms, but as soon as it is transmitted to humans becomes critical and severe to the extent of fatal. The mortality rate especially in the second week of infection reaches to approximately 30% (14, 4). Due to the lack of complete knowledge of the CCHF infection epidemiology in Iraq and because of the widespread infection of animals carrying different tick species, the current study hypothesized that viral infections are likely to be transmitted to humans. Thus, the current study aimed to investigate the CCHF morbidity and mortality rate in Iraqi communities.
Ethics Considerations
Prior approval was obtained from the Scientific Research Ethics Committee at the Faculty of Education for Pure Sciences / University of Diyala (CEPC/112-5/5/2021) to conduct the research project after scientific review by the members of the scientific committee and in cooperation with the Ministry of Health.
Study populations
The current study was conducted in cooperation with the health departments from 8 Iraqi governorates; Dhi Qar, Baghdad, Nineveh, Babel, Erbil, Diyala, Anbar and Muthanna. A total of 61 samples reserved from the patients suspected of having CCHF infection who attended health department from May to December 2021 were included. Demographic data such as age, sex, and area of residence were collected from the records. The specimens were promptly dispatched to the Central Public Health Laboratory in Baghdad and managed in biohazard conditions of utmost biological containment. A molecular detection test was performed on the saved blood samples to diagnose CCHFV.
Molecular Detection
The genomic RNA was extracted from the samples using QIAamp viral RNA mini kit (QIAGEN, Germany) according to the manufacturer’s instructions. The viral RNA was kept at -80°C for furtherexamination by the real-time reverse transcriptase-PCR (rRT-PCR). The yield of viral RNA was analyzed by a detection kit (the RealStar® CCHFV RT‒PCR Kit 1.0; Altona Diagnostics GmbH, Germany). The amplification procedure included the following steps: a specific cycle of reverse transcription-holding at 50°C for 10 min, followed by denaturation at 95°C for 2 min and 45 cycles of amplification at 95°C for 30 sec, 55°C for 30 sec, and 72°C for 30 sec using thermal cycler (QuantStudioTM 5 Real-Time PCR system). Positive results were found through the use of fluorescence detector dyes (CCHF-specific RNA CCHFV FAMTM). The rRT-PCR test offered the highest level of sensitivity for detecting active infections.
Statistical Analysis
To manage and analyze the frequencies, percentages and specific graphs, the statistical software packages GraphPad Prism 8.0.0 and SPSS Statistics 25.0/IBM Crop., Armonk, NY were used. To characterize the median with a specific interquartile range, the normality test was used for ongoing variables. When distribution of the data was not normal the Kruskal– Walli’s test was used. Pearson's chi-square test was used to compare the variables. To be statistically significant P-value was considered less than 0.05.
The results of CCHF RNA detection for a total of 61 samples with suspected symptoms of CCHF infection showed 18 (29.5%) positive for the presence of the virus, and 8 (44.44%) of these positive patients died following the infection. These two groups of patients showed significant difference (chi-square = 10.25; P<0.01) as shown in Table 1.
Table 1. Positive and negative rates of CCHF virus infection
| PCR result | N | Minimum | Maximum | Mean ± SD |
| Negative | 43 | 9 | 80 | 38.63 ± 18.264 |
| Positive | 18 | 16 | 60 | 32.06 ± 14.198 |
A comparison between the incidences of positive cases and deaths among the ≤40 years and >40 years age groups showed that both the positive cases and deaths were significantly greater among the ≤40 years age group (chi-square = 5.56; P<0.05) (Figure 1).
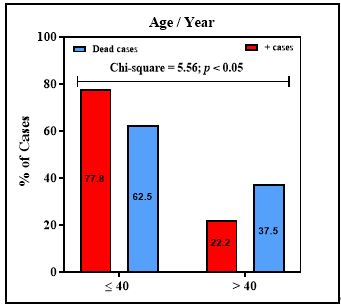
Figure 1. Distribution of CCHF positive rate and death according to the age group
Table 2. Distribution of CCHF infection by month of the year
| Month | Positive cases No. (%) |
Negative cases No. (%) |
Chi-square = 2.89; P-value= 0.409 NS |
| May | 0 | 1 (2.3%) | |
| June | 1 (5.6%) | 7 (16.3%) | |
| July | 2 (11.1%) | 7 (16.3%) | |
| August | 0 | 1 (2.3%) | |
| September | 7 (38.9%) | 10 (23.3%) | |
| October | 1 (5.6%) | 4 (9.3%) | |
| November | 5 (27.8%) | 8 (18.6%) | |
| December | 2 (11.1%) | 5 (11.6%) | |
| Total | 18 (29.5%) | 43 (70.5%) |
Table 3. Distribution of CCHF infection according to DOH in different Provinces
| Province | Positive cases No. (%) |
Negative cases No. (%) |
Chi-square = 16; P-value<0.001 HS |
| Dhi Qar | 14 (77.8%) | 29 (67.4%) | |
| Baghdad | 0 | 4 (9.3%) | |
| Nienwa | 2 (11%) | 3 (6.9%) | |
| Babil | 0 | 2 (4.7%) | |
| Erbil | 0 | 4 (9.3%) | |
| Diayla | 1 (5.6%) | 0 | |
| Anbar | 0 | 1 (2.3%) | |
| Muthana | 1 (5.6%) | 0 | |
| Total | 18 (29.5%) | 43 (70.5%) |
During the period of COVID-19 outbreak all over the world and Iraq in particular, a decline in monitoring and treatment procedures from the veterinary side regarding the infection of animals with disease-causing ticks was observed. This led to an increase in the incidence of CCHF outbreaks during the year of the study period (2021) and beyound, as shown by different reports from media and WHO (15, 16). The other reason for continuous spread of CCHFV outbreaks in Iraq might be for the religious celebrations such as Eid al-Adha that many people keep livestock at home to sacrifice them during the feasting ceremony. In addition, slaughtering procedures that are not subject to the health control and proper handling of the waste material of these animals, such as blood and skin, may be another important reason for the transmission of this virus to people (17).
Therefore, the health departments in the governorates of Iraq commenced to conduct epidemiological examinations with WHO support by providing diagnostic kits and laboratory equipment (18). Molecular diagnostic examination on the saved samples from May to December 2021 in Iraq showed confirmed positive cases and deaths with CCHFV infection at 18 (29.5%) and 8 (44.44%), respectively. Since then, confirmed cases increased subsequently according to WHO reports (12) and subsequent studies (16, 19). Based on these studies, a total of 212 cases of CCHF and 27 deaths were reported. Of these, 97 cases, representing 46%, were confirmed by RT-PCR, while the remaining 115 cases, representing 54%, were considered suspected. The majority of the reported human cases were associated with individuals involved in livestock farming and meat processing such as butchers (16, 19).
A risk factor that increases the incidence of CCHF infection is the increasing prevalence of ticks. Geographically, Iraq is one of the countries that are endemic to CCHFV. Previous outbreaks with similar characteristics have been observed in Iraq (20, 21). Turkey is also endemic to CCHF infection. In a study by Tartar et al. (22), most of the individuals with CCHF were males, and this was confirmed by a study conducted in Iraq (16), which is not consistent with the results of the present study. The increase in positive cases of infection and death, as shown in the present study, was observed among the ≤ 40 years age group. This was confirmed by previous studies, as the highest infection rate was in males aged less than 40 years. The high infection rate among these age groups may have several reasons, including the higher number of suspects diagnosed within that age group, as well as the increased social activities of those age groups and their frequent contact with the virus, particularly among those working in slaughtering houses and processing leather (15, 23, 24). Dhi Qar Governorate recorded the highest rate of CCHF infection during the study period in 2021, during which the disease was recorded as the most common infection. According to the local reports and WHO, documented on December 16, 2022 (18), Dhi Qar province was still recording a continuous infection with the virus.
The number of CCHF infections in rural areas (25, 26), where the numbers of domestic and wild animals as vectors of CCHFV are high may deteriorate the health and economic reality in the governorates of southern Iraq.
Several international studies indicate the presence of 28 different types of ticks, but no epidemiological survey studies have been conducted at the level of Iraq (8, 27, 28). An Iranian study of the tick parasites in Iran-Iraq border strip showed a high prevalence of ticks among sheep and cattle (29). In North Africa and the Arabian Peninsula, a total of 55 tick species belonging to the eight livestock species have been documented (30). Health awareness campaigns, correct handling of animals before slaughtering, and having personal protective equipment (PPE) may play major roles in reducing the infection rates.
It is essential to note that one of the most important constraints the current study faced with was the small sample size, due to the fact that the period of conducting this study was at the same time of the height peak of the COVID-19 pandemic, which pandemic situation was more focused at that time.
Although the number of studied cases was relatively small and may not generalize the broader situation of CCHF in Iraq, it can be considered a health concern in the region. Therefore, there is an urgent need to conduct epidemiological surveys in cooperation with global health authorities to reduce the infection rates and detect the extent of the ticks spread that are vectors of the virus. The current study recommends intensifying efforts by the country's health authorities and introducing new policies to reduce the recurrence of the outbreak in the country, this pattern was sensitive and intermediate, respectively.
The researchers would like to thank all colleagues involved in this project progress.
Ethical Considerations
Prior approval was obtained from the Scientific Research Ethics Committee at the Faculty of Education for Pure Sciences / University of Diyala (CEPC/112-5/5/2021) to conduct the research project after scientific review by the members of the scientific committee and in cooperation with the Ministry of Health.
Authors’ Contributions
Conceptualization and data curation: Hula Y. Fadhil and Iman M. Aufi, Methodology: Raghad. I. Khaleel, Noora. A. Abdulhadi, Ahmed, A. Hussein, Ihab. R. Aakef, Project administration: Asmaa Haseeb Hwaid, Resources: Ahmed, A. Hussein, Ihab. R. Aakef, Validation: Asmaa Haseeb Hwaid, Writing–original draft: Asmaa Haseeb Hwaid, Writing–review & editing: Asmaa Haseeb Hwaid, Hula Y. Fadhil and Iman M. Aufi.
Researchers did not receive financial support for conducting this study.
Conflicts of Interest
Conflicts of Interest
WHO: World Health Organization
CCHF: Crimean-Congo hemorrhagic fever.
Received: 2024/07/2 | Accepted: 2024/09/12 | ePublished: 2024/09/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





