BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-2384-en.html


 , Armin Shalchian2
, Armin Shalchian2 

 , Gholamreza Irajian3
, Gholamreza Irajian3 

 , Hamidreza Sadeghsalehi4
, Hamidreza Sadeghsalehi4 

 , Abed Zahedi bialvaei5
, Abed Zahedi bialvaei5 

 , Babak Sabet6
, Babak Sabet6 


2- Department of Computer Engineering, West Tehran Branch, Islamic Azad University, Tehran, Iran
3- Microbial Biotechnology Research Center, Iran University of Medical Sciences, Tehran, Iran & Department of Microbiology, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran
4- Department of Neuroscience, Faculty of Advanced Technologies in Medicine, Iran University of Medical Sciences, Tehran, Iran
5- Microbial Biotechnology Research Center, Iran University of Medical Sciences, Tehran, Iran
6- Faculty of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran & Department of Artificial Intelligence, Smart University of Medical Sciences, Tehran, Iran
Antimicrobial resistance (AMR) poses a global health crisis wherein microorganisms like bacteria, viruses, fungi, and parasites develop resistance to antimicrobial drugs, diminishing their effectiveness in treating infections (1). This resistance jeopardizes the potency of antibiotics, antivirals, and antifungals, crucial for combating infectious diseases and upholding public health. The proliferation of AMR carries profound consequences for healthcare systems on a global scale. The World Health Organization (WHO) reports that AMR leads to approximately 700,000 deaths annually, and if unchecked, this figure could escalate to 10 million deaths yearly by 2050, accompanied by a cumulative economic burden of $100 trillion (2). AMR not only increases the morbidity and mortality rates associated with infections but also contributes to prolonged hospital stays, increased healthcare costs, and reduced treatment options. It poses a particular risk to vulnerable populations, such as the elderly, newborns, and individuals with compromised immune systems (3, 4). The global impact of AMR extends beyond human health and affects veterinary medicine, agriculture, and food production due to the widespread use of antimicrobials in these sectors. AMR development and spread are fueled by the misuse and overuse of antimicrobials in humans and animals, coupled with inadequate infection prevention and control practices. Conventional drug discovery struggles to keep up with the rapid emergence of AMR, resulting in a limited pipeline of new antimicrobial agents. Therefore, addressing the multifaceted challenge of AMR requires a multidisciplinary approach and innovative strategies and technologies to ensure effective treatments for infectious diseases.
The need for innovative approaches in drug discovery arises from the scarcity of new antibiotics to combat the growing threat of AMR. The traditional drug discovery process, which relies on screening natural products and making chemical modifications, has fallen behind the rapid emergence of resistant bacteria. The high failure rates and long timelines associated with antibiotic development have discouraged pharmaceutical investment in this area (5).
Given this context, innovative approaches are essential to overcome AMR challenges and maintain a sustainable arsenal of effective antimicrobial agents. These approaches aim to identify new targets, develop novel compounds, and optimize existing antibiotics against resistant pathogens.
The integration of advanced technologies, such as artificial intelligence (AI), offers promising opportunities in drug discovery, surveillance, diagnostics, and personalized medicine.
This narrative review explores the integration of AI into drug discovery and development to combat antimicrobial resistance. It examines various AI applications in target identification, compound screening, lead optimization, and repurposing. The review also discusses the challenges and limitations associated with AI in AMR-focused drug discovery, as well as ethical considerations. By harnessing the potential of AI, it becomes possible to expedite the discovery of novel antimicrobial agents, optimize existing drugs, and effectively combat the growing threat of antimicrobial resistance.
-
-
Motivation
-
Several studies have extensively explored the applications of AI and machine learning (ML) in the analysis of data for drug discovery and development (6, 7). However, a noticeable gap exists in research concerning the utilization of AI in the specific domain of Antimicrobial Resistance, unlike the comprehensive studies in drug development. This gap in the literature has prompted the researchers of this manuscript to conduct a Narrative Review, filling the void and laying the groundwork for future studies in this crucial field. The aim is to contribute valuable insights to scientific communities and stimulate further exploration into the potential of AI in combating Antimicrobial Resistance.
-
-
AI Discipline and methods of AI
-
In recent years, there has been a significant rise in the digitalization of data within the pharmaceutical sector. However, this digital transformation poses challenges in terms of acquiring, analyzing, and effectively applying knowledge to address intricate clinical issues. This has led to a growing interest in the use of AI due to its ability to handle substantial amounts of data through improved automation. AI, as a technology-based system, incorporates various advanced tools and networks that emulate human intelligence without completely replacing human physical presence (8). AI employs systems and software capable of interpreting and learning from input data to autonomously make decisions in pursuit of specific objectives. The applications of AI in the pharmaceutical field are continually expanding, as discussed in this review. According to the McKinsey Global Institute, the swift progress in AI-guided automation is poised to bring about profound changes in societal work culture (9).
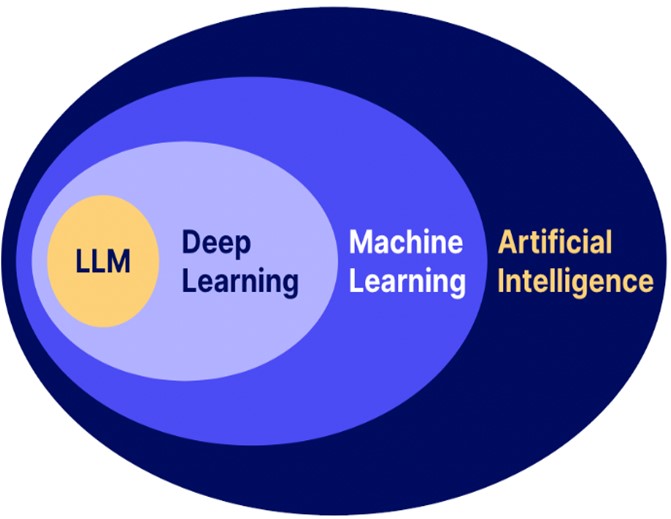
AI encompasses various methodological domains, including reasoning, knowledge representation, solution search, and, notably, a fundamental paradigm known as ML, Deep Learning (DL) and Language large models (Figure 1).
ML employs algorithms capable of identifying patterns within categorized datasets. Within ML, there exists a subfield known as deep learning, which employs artificial neural networks (ANNs) (10). These networks consist of interconnected sophisticated computing elements resembling human biological neurons, imitating the transmission of electrical impulses in the human brain. ANNs consist of nodes, each receiving distinct inputs and ultimately producing outputs, either individually or through multilinked configurations, utilizing algorithms to address problems (11). There are various types of ANNs, such as multilayer perceptron (MLP) networks, recurrent neural networks (RNNs), and convolutional neural networks (CNNs), which employ either supervised or unsupervised training procedures (12).
Figure 1. The Discipline of AI subdivision and methods (Designed by Authors, 2024)
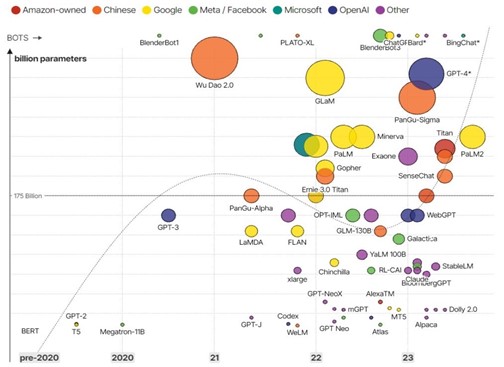
Over the past one or two years, a transformative concept has surfaced, signifying a notable shift in the realm of artificial intelligence—namely, the emergence of generative AI networks. The core of this Generative AI concept lies in Large Language Models (LLMs), sparking significant transformations at the peripheries of applied knowledge (13). In recent months, there has been a pronounced surge in innovative developments within the field of generative artificial intelligence, particularly with the widespread attention garnered from academic, media, and public spheres. Prominent examples of LLMs include GPT-3, BERT, and ChatGPT, all of which have undergone extensive training on vast portions of the internet, resulting in their ability to generate impressive responses to human queries (14). The versatility of these generalized LLMs extends to tasks such as fiction writing, computer code development, and speculative discussions about the future, prompting the acknowledgment that we are on the brink of achieving artificial general intelligence for the first time. The figure (2) illustrates the LLMs developed in the recent months.
Figure 2. The LLM based technologies and Chatbot (Designed by Authors, 2024)
The information obtained to write this study was collected from reliable databases including Scopus, PubMed and Google Scholar.
In this investigation, we reviewed pertinent research in the scientific database, assessed the strengths and weaknesses of traditional approaches in drug development, categorized diverse artificial intelligence applications within the field of drug development, and conducted a thorough analysis of drug discovery methods, placing specific emphasis on addressing Antimicrobial Resistance.
3.1 Conventional Drug Discovery Approaches and Limitations
Conventional drug discovery approaches have played a vital role in the development of various antimicrobial agents. However, these approaches face several limitations, resulting in challenges in combating AMR. Phenotypic screening involves testing compounds for their ability to produce a desired biological effect in whole organisms or cells. This approach allows for the identification of compounds with desired activity but without the need for prior knowledge of the target. However, phenotypic screening often lacks mechanistic insights, making it challenging to optimize compounds or understand their specific mode of action (15). Additionally, the identification of the target can be laborious and time-consuming. On the other hand, target-based screening focuses on identifying compounds that interact with a specific target, such as a protein or enzyme involved in a disease pathway. This approach relies on knowledge of the target's structure and function. However, the identification of suitable targets can be difficult, particularly in complex diseases with poorly understood mechanisms (16). Moreover, the reliance on single targets may overlook the complexity of disease biology and the potential for compensatory mechanisms.
Combinatorial chemistry is another conventional drug discovery approach that involves the synthesis and screening of large libraries of compounds with diverse structures (17). This approach aims to explore a wide chemical space and identify compounds with desired biological activity. However, the sheer size of compound libraries makes screening and optimization challenging, as it requires significant time, resources, and expertise (18). Furthermore, combinatorial chemistry may not adequately explore the chemical diversity needed to address complex targets or pathways.
Natural products have served as a valuable source of drug leads. Extracts from plants, microbes, and marine organisms have historically provided numerous bioactive compounds. However, the process of discovering and isolating natural products can be labor-intensive and time-consuming (19). Additionally, the limited supply and challenges in scaling up production have posed obstacles to their development as drugs. An essential aspect of drug discovery is ensuring that compounds have desirable pharmacokinetic properties, such as bioavailability, appropriate half-life, and metabolic stability. Furthermore, compounds must undergo rigorous safety assessments to determine their potential toxicity and side effects. These factors add to the complexity and cost of drug discovery, as compounds must meet stringent criteria for further development (20).
The challenges associated with traditional drug discovery methods have led to an increased interest in innovative approaches, such as AI, machine learning, and computational modeling, to overcome these limitations. By leveraging these technologies, researchers can analyze large datasets, model complex interactions, and design more efficient and targeted drug discovery strategies.
-
- Crucial Role of AI in Tackling the AMR
AMR in bacteria is a global health crisis due to the rapid emergence of multidrug-resistant bacteria and the protracted development of new antimicrobials. The rise of AMR in bacteria since the 1940s has become a global health crisis (21). AMR develops through genetic mutation and spreads naturally through horizontal gene transfer. The long process of discovering and developing antimicrobials, including years of clinical trials, contrasts with the misuse and easy accessibility of antibiotics, leading to multidrug resistance (MDR) (22, 23). This crisis has resulted in a shortage of safe antimicrobials to combat MDR bacteria. To address this, rapid and efficient identification of bacterial AMR is crucial. AI, particularly ML, emerges as a novel approach for accurate and timely identification. ML involves training computers with large sets of experimental data. Databases like CARD and MegaRES collect peer-reviewed AMR determinants data, enabling the training of algorithms to reliably identify known or novel AMR and predict minimum inhibitory concentrations of MDR bacteria. This AI-based approach aims to combat the global AMR crisis and reduce antimicrobial misuse (24).
AI techniques have shown great potential in transforming various aspects of drug discovery and development. By leveraging large-scale genomic, proteomic, and metabolomic data, AI algorithms can aid in target identification, compound optimization, and prediction of antimicrobial resistance patterns (25, 26). These AI-driven approaches provide researchers with valuable insights, enabling them to make informed decisions and prioritize resources effectively.
Furthermore, AI can facilitate the repurposing of existing drugs for antimicrobial use, allowing for a more rapid and cost-effective development process. Drug repurposing, combined with AI techniques, can help identify non-antibiotic compounds that possess antimicrobial activity, potentially expanding the repertoire of available treatments (27). This approach can offer a valuable alternative to traditional antibiotic development and overcome some of the challenges associated with de novo compound discovery.
The significance of innovative approaches in drug discovery extends beyond the development of new antimicrobial agents. It also encompasses the optimization of existing antibiotics to enhance their efficacy, minimize toxicity, and combat resistance mechanisms. AI-driven computational approaches, such as structure-based drug design and virtual screening, can facilitate the modification and optimization of antibiotic compounds, improving their pharmacological properties and reducing the likelihood of resistance development (28).
3.3 AI Applications in AMR
3.3.1 Traditional Machine learning in identifying antimicrobial compounds
Machine learning, a subset of artificial intelligence, has emerged as a powerful tool in drug discovery, including the identification of antimicrobial compounds. By leveraging large datasets, computational algorithms, and pattern recognition, machine learning techniques contribute to the rapid and efficient identification of potential antimicrobial agents. This section explores the role of machine learning in identifying antimicrobial compounds and provides relevant references supporting its application.
1. Data-driven Approaches: Machine learning algorithms can analyze vast amounts of data, including chemical structures, biological activity profiles, and genomic information, to identify patterns and relationships associated with antimicrobial activity. By learning from existing data, machine learning models can predict the antimicrobial potential of novel compounds and prioritize candidates for further experimental validation (26, 29).
2. Virtual Screening and Drug Repurposing: Machine learning techniques enable virtual screening, a computational approach used to identify potential antimicrobial compounds from large chemical libraries. By training models on known antimicrobial compounds and their properties, machine learning algorithms can efficiently screen millions of compounds and rank them according to their likelihood of exhibiting antimicrobial activity. Furthermore, machine learning can aid in drug repurposing, identifying existing drugs with potential antimicrobial properties (30, 31).
3. Feature Extraction and Descriptors: Machine learning models require informative features or descriptors to capture the relevant characteristics of antimicrobial compounds. Various molecular descriptors, including physicochemical properties, molecular fingerprints, and structural fragments, can be used as input features for machine learning algorithms. These descriptors help in representing the compounds' chemical space and facilitate the prediction of their antimicrobial properties (32, 33).
4. Predictive Models and Optimization: Machine learning algorithms can build predictive models that classify compounds as antimicrobial or non-antimicrobial based on their features. These models can be trained on labeled datasets and optimized to improve their accuracy and generalizability. Additionally, machine learning can aid in optimizing the chemical structures of compounds to enhance their antimicrobial activity through virtual screening and molecular design (25, 34).
5. Antibiotic Resistance Prediction: Machine learning techniques can also be employed to predict and analyze antibiotic resistance. By analyzing genomic data from resistant strains, machine learning models can identify genetic markers and patterns associated with resistance mechanisms. This information can guide the development of novel antimicrobial compounds or strategies to combat resistance (35, 36).
3.3.2. Deep learning for drug design and optimization
Deep learning models can generate novel compounds with desired properties by learning patterns from large chemical databases. Generative models, such as generative adversarial networks (GANs) and variational autoencoders (VAEs), can produce structurally diverse compounds with specific chemical characteristics. These generated compounds can serve as starting points for further optimization and synthesis (37, 38).
Deep learning algorithms can accurately predict various molecular properties, such as solubility, bioactivity, toxicity, and binding affinity. By training on large datasets of chemical structures and their corresponding properties, deep learning models can learn complex relationships and make predictions on new compounds. These predictions aid in prioritizing compounds for synthesis and screening, thereby saving time and resources (39, 40). Deep learning models can also be employed for virtual screening, which involves computationally screening large compound libraries to identify potential hits against specific targets. CNNs and RNNs can analyze molecular structures, protein-ligand interactions, and binding affinities to rank compounds based on their likelihood of binding to a target. This approach helps in identifying promising lead compounds for further experimental validation (41, 42).
Deep learning techniques enable de novo drug design, where the algorithm generates novel compounds with optimized properties. By incorporating desired molecular properties, constraints, and target interactions into the model, deep learning algorithms can explore the chemical space and propose compounds with improved efficacy and reduced off-target effects (43, 44). Additionally, deep learning algorithms can analyze large-scale biological and chemical data to identify new therapeutic indications for existing drugs. By integrating diverse datasets, such as gene expression profiles, drug-protein interactions, and disease networks, deep learning models can predict potential drug-disease associations and repurpose approved drugs for new indications (45, 46).
3.3.3 LLM in Drug discovery and development
Due to the novelty of this technology, its applications in the field of drug discovery and development have not been developed much. But this field has great potential in the development of new and recombinant drug structures. This interactive technology is able to provide constructive suggestions with the researchers of this field based on the topics that the model has learned on. LLM in Drug Discovery and Development can be a valuable tool in various aspects of the drug development process. But five accepted uses of an LLM can be listed and categorized by reviewing the research done (47, 48). A) Drug design and optimization: LLMs can generate new drug structures by inferring missing protein segments or small molecule sequences. These models can quickly generate new structures that can potentially be useful in drug development. B) Toxicity prediction: LLMs can be used to score new drug structures with respect to toxicity. By analyzing the generated structures, LLMs can provide insight into the potential toxicity of a drug candidate. C) Binding affinity prediction: LLMs can also predict the binding affinity of a drug candidate to its target protein. This information is very important in determining the effectiveness of a drug in interaction with its target and can help to optimize drugs. D) Ease of Synthesis Prediction: LLMs can assess the ease of synthesis of a drug candidate. This information is important in determining the feasibility and cost-effectiveness of large-scale production of a drug. E) Predicting pharmaceutical similarity: LLMs can evaluate the pharmaceutical similarity of a compound by considering various factors such as molecular weight, lipophilicity, and structural features. This evaluation helps identify compounds with a higher probability of success in drug development. It is noteworthy that while LLMs can generate new drug structures and provide predictions, further validation and experimental testing are necessary to confirm the efficacy and safety of these candidates.
3.3.4. Data mining and knowledge discovery in AMR databases
Data mining and knowledge discovery techniques play a crucial role in extracting valuable insights and patterns from large-scale AMR databases. By applying computational methods and statistical analysis to these databases, researchers can uncover hidden relationships, identify emerging resistance patterns, and guide the development of effective strategies to combat AMR. Data mining algorithms can identify patterns and clusters within AMR databases, enabling the discovery of novel resistance mechanisms and the characterization of resistance profiles. By analyzing large collections of microbial genomes and resistance phenotypes, clustering techniques, such as k-means clustering and hierarchical clustering, can group similar strains based on their resistance patterns and identify outliers with unique AMR characteristics (49, 50).
Association rule mining techniques, such as Apriori and FP-growth, can uncover associations and correlations between different antimicrobial resistance genes, mutations, and phenotypes. By analyzing AMR databases, these algorithms can identify co-occurring resistance genes or mutations, providing insights into the genetic determinants of resistance and potential gene interactions (51, 52). In addition, data mining approaches can build predictive models to forecast antimicrobial resistance based on various factors, including genomic data, patient demographics, and environmental conditions. Machine learning algorithms, such as decision trees, support vector machines (SVM), and random forests, can learn from historical data to predict the likelihood of resistance emergence or the effectiveness of specific antimicrobial treatments (53, 54). Network analysis techniques, such as graph theory and network clustering, can also reveal the complex relationships between AMR genes, mobile genetic elements, and bacterial strains. By constructing networks based on gene co-occurrence or genetic similarity, these methods can identify key resistance genes, transmission routes, and potential sources of resistance dissemination (55, 56).
Text mining and natural language processing techniques can extract valuable information from scientific literature, clinical reports, and other textual sources related to AMR. By analyzing and categorizing text data, these methods can identify novel resistance mechanisms, track the spread of specific resistance genes, and facilitate the curation and integration of AMR knowledge (57, 58).
3.3.5 Extra application of AI in combating AMR
3.3.5.1 AI in High-Throughput Screening, Genomics, and Proteomics
High-throughput screening (HTS), genomics, and proteomics are essential fields in drug discovery and biomedical research. The integration of AI into these fields has revolutionized the way scientists analyze and interpret large-scale biological data, leading to more efficient and accurate results. Research has demonstrated that AI has sparked innovation in various areas, including high-throughput screening, genomics, and proteomics.
3.3.5.2 Genomics analyzer equipped with AI
AI algorithms can analyze large-scale genomic data, including DNA sequencing and gene expression data, to identify patterns and associations that may be relevant to disease diagnosis, prognosis, and treatment. AI can help interpret genomic variants and help researchers identify disease-causing mutations and potential therapeutic targets. AI can predict gene functions and regulatory elements based on genomic data and help to understand gene networks and biological processes (59).
3.3.5.3 Proteomics Analyzer Equipped with AI
AI algorithms can analyze proteomics data, such as protein expression levels and post-translational modifications, to identify biomarkers for disease diagnosis, prognosis and treatment. AI can predict protein structures and interactions and help to understand protein function and drug-target interactions. AI can help identify potential drug targets by analyzing proteomics data and identifying proteins involved in disease pathways. Overall, the integration of AI into high-throughput screening, genomics, and proteomics has significantly increased the efficiency and accuracy of data analysis, leading to improved drug discovery findings and biomedical research outcomes (60).
3.3.5.4 Accelerating drug discovery through AI-powered screening
AI-powered screening methods leverage ML algorithms to analyze large datasets, predict compound properties, and prioritize molecules for further experimental validation. This section discusses the applications of AI-powered screening in drug discovery, supported by relevant references.
1. Virtual Screening: AI algorithms can perform virtual screening to computationally evaluate large libraries of compounds and identify potential drug candidates. Machine learning models, such as SVM, random forests, and deep learning architectures, can analyze molecular structures, physicochemical properties, and biological data to predict the likelihood of a compound's activity against a specific target. This approach helps in prioritizing compounds for experimental testing, reducing the time and cost associated with traditional screening methods (61, 62).
2. HTS Data Analysis: AI algorithms can analyze data generated from high-throughput screening campaigns, where thousands of compounds are tested against a target in a short period. By applying machine learning techniques, such as clustering, classification, and regression, to HTS data, AI models can identify active compounds, understand structure-activity relationships, and predict the potency of untested compounds. This enables researchers to make informed decisions and focus on the most promising molecules (26, 63).
3. De Novo Design: AI-powered approaches facilitate de novo drug design by generating novel compound structures with desired properties. Generative models, including generative adversarial networks (GANs) and variational autoencoders (VAEs), can learn from existing compound libraries and generate new molecules with optimized properties. By combining generative models with reinforcement learning techniques, AI algorithms can iteratively design and refine compounds based on target interactions and desired drug properties (38, 43).
4. Drug Repurposing: AI algorithms can mine large-scale biological and clinical datasets to identify potential new applications for existing drugs. By integrating diverse data sources, such as genomic data, electronic health records, and drug databases, AI models can predict novel drug-disease associations and repurpose approved drugs for new indications. This approach allows for the rapid identification of potential therapeutic options and reduces the time and cost required for preclinical and clinical development (64, 65).
5. Predictive ADME-Tox Modeling: AI techniques can predict the absorption, distribution, metabolism, excretion, and toxicity (ADME-Tox) properties of compounds. By training on large datasets of compound properties and experimental data, AI models can predict the pharmacokinetic and toxicological profiles of new compounds. This helps in identifying potential safety concerns and optimizing lead compounds early in the drug discovery process (66, 67).
3.3.5.5 Utilizing genomics and proteomics data for AMR prediction
Genomics and proteomics data provide valuable insights into the genetic and molecular mechanisms underlying AMR. By analyzing genomic sequences and proteomic profiles of microbial strains, researchers can identify genetic markers, resistance genes, and molecular pathways associated with AMR. Genomic data, including whole-genome sequencing (WGS) and metagenomic sequencing, can provide insights into the genetic basis of AMR (68). By comparing the genomic sequences of resistant and susceptible strains, researchers can identify genetic variations, mutations, and mobile genetic elements associated with resistance. Bioinformatics tools and machine learning algorithms can analyze these genomic features to predict the likelihood of AMR and guide treatment decisions (69, 70).
The resistome refers to the collection of all resistance genes present in microbial genomes or metagenomic samples (71). HTS technologies enable researchers to profile the resistome and identify the repertoire of resistance genes within a microbial community. By analyzing the resistome, researchers can predict the potential resistance phenotypes and monitor the spread of resistance genes in various environments (72, 73). In addition, transcriptomic analysis, such as RNA sequencing (RNA-seq), can provide insights into the gene expression patterns associated with AMR. By comparing the transcriptomes of resistant and susceptible strains, researchers can identify differentially expressed genes and pathways involved in resistance mechanisms. This information can be used to predict AMR phenotypes and understand the regulatory networks underlying resistance (74, 75). Proteomics data can also contribute to AMR prediction by characterizing the protein expression profiles of resistant strains. Mass spectrometry-based proteomics enables the identification and quantification of proteins involved in resistance mechanisms. By comparing the proteomes of resistant and susceptible strains, researchers can identify differentially expressed proteins, post-translational modifications, and protein-protein interactions related to AMR (76, 77).
Integration of genomics, transcriptomics, proteomics, and other omics data can provide a comprehensive view of AMR mechanisms. By combining multiple layers of molecular information, researchers can identify key genetic variations, gene expression patterns, and protein interactions contributing to resistance. Integrated omics approaches, along with advanced data integration and machine learning techniques, can enhance AMR prediction and facilitate the development of personalized treatment strategies (78, 79).
3.3.5.6 AI-guided approaches for personalized medicine in AMR
AI plays a crucial role in advancing personalized medicine approaches for AMR. By leveraging AI algorithms, researchers can analyze diverse patient data, including genomics, clinical information, and microbial profiles, to develop tailored treatment strategies for individuals. AI algorithms can analyze genomic data, such as WGS or metagenomic sequencing, to identify genetic markers and resistance mechanisms associated with AMR. By integrating genomic information with clinical data, AI models can aid in precise diagnosis, determining the most effective antimicrobial treatment based on the patient's genetic profile (80, 81).
AI models can utilize machine learning techniques to analyze clinical and microbiological data to predict treatment outcomes for AMR infections. By incorporating features such as patient demographics, comorbidities, antimicrobial resistance profiles, and treatment regimens, AI algorithms can help clinicians make informed decisions about the most suitable antibiotic therapy for individual patients (82, 83). AI-based models can analyze patient-specific data, including drug concentrations, pharmacokinetics, and clinical parameters, to optimize antimicrobial dosing through TDM. These models can help clinicians adjust dosages in real-time to ensure therapeutic efficacy while minimizing toxicity and the development of resistance (84, 85).
AI-powered decision support systems can integrate patient data, clinical guidelines, and expert knowledge to assist healthcare providers in selecting the most appropriate antimicrobial treatment (86). These systems can aid in decision-making by considering factors such as resistance patterns, individual patient characteristics, and local epidemiology (87). AI algorithms can also analyze large-scale, real-time data from electronic health records, laboratory records, and public health databases to detect AMR trends and outbreaks (88). By identifying patterns and anomalies, AI models can facilitate early detection, enabling timely intervention and the implementation of appropriate infection control measures (89).
The application of AI in combating AMR within drug discovery and development shows significant potential in addressing the global AMR challenge. This narrative review underscores the capabilities of AI across different phases of the drug discovery and development continuum, encompassing target identification, lead optimization, and the prediction of drug resistance. Various studies have validated the efficacy of AI-based approaches in identifying new antimicrobial compounds and enhancing existing drugs to combat AMR. Furthermore, AI demonstrates promise in forecasting drug resistance and guiding personalized treatment strategies. Despite notable advancements in this domain, there exist challenges and limitations that warrant attention. Additionally, ensuring the interpretability and explainability of AI models remains pivotal, particularly in the context of regulatory approval and clinical implementation.
We appreciate our colleagues in the Department of Microbiology of Iran University of Medical Sciences. In addition, we have a special thanks to Engr. Amirhossein Chehrehara who helped us in publishing this article.
Ethical Approval
Not applicate.
Authors’ Contributions
A.Z.B designed the study; M.G., A.S., A.Z.B. and H.S. collected data and prepared Manuscript draft; A.Z.B. and M.G. directed and managed the study; G.I. and B.S. revised critically and edited the manuscript. All authors studied and approved the final manuscript.
The author(s) received no financial support for the research or publication of this article.
Conflicts of Interest
No conflicts of interest were declared by the authors.
Received: 2024/04/27 | Accepted: 2024/07/17 | ePublished: 2024/08/18
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |