BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-2184-en.html
2- Department of Microbiology, Faculty of Life Sciences, Islamic Azad University, Parnad Branch, Tehran, Iran
3- Department of Microbiology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran ,
Mycobacterium tuberculosis (M. tuberculosis) is a non-motile, non-spore-forming, obligate aerobe, acid-fast bacilli with specific cell wall, which is named “king of bacteria” by microbiologists. Most patients are asymptomatic during the incubation period with no radiologic signs of disease; although they develop cell-mediated immunity and tests of tuberculosis (TB) infection can become positive by tuberculin skin test and the interferon-γ release in 40-50% of the patients (1).
M. tuberculosis is the second most fatal infection after HIV (AIDS) and is important subject for the global health. According to the latest researches and World Health Organization (WHO) reports, one-third of the world's population has been infected with this bacterium and immediate detection of M. tuberculosis could prevent the spread of the disease (2). The traditional diagnostic tests for TB such as chest X-ray, culture, tuberculin skin test (TST), and acid-fast staining have so many limitations. Chest X-ray is insufficient and the culture although is considered as a gold standard method recommended by WHO for the diagnosis of tuberculosis, takes too long. The TST lacks specificity and reliability and the acid-fast staining depends on a large number of bacteria in the sputum to give an accurate reading.
Serological tests, using different TB antigens to detect M. tuberculosis infection, are fast but lack the desired sensitivity. Although new methods such as nucleic acid amplification technology (NAAT) has specificity, it can yield false-positive results. Immunologic tests (QuantiFERON and T-SPOT.TB), which measure the production of IFN-γ by TB-specific T lymphocytes after encountering M. tuberculosis antigens, have certain advantages over the conventional tests, but they have disadvantages as well (3).
According to the above explanation, a cost-effective, accurate, and rapid method of diagnosis for both active and latent TB infections is recommended (4). The molecular techniques provide faster and more accurate detection of MTB complex from respiratory and extra-pulmonary specimens (5). The rapid detection of rifampin (RIF)-resistant M. tuberculosis in infected patients is essential for the disease management, because of the high risk of transmission from person to person and emergence of the resistant strains such as MDR and extensively drug resistant (XDR) tuberculosis. The NAAT is essential for earlier treatment initiation and more effective public health interventions (6). Although, both M. tuberculosis (MTB) and non-tuberculosis mycobacteria (NTM) species have common clinical signs, they should be distinguished from each other. Biochemical tests are used to differentiate MTB from NTM. In 1995, the amplified mycobacterium direct test was the first standard nucleic acid based amplification test used by the organizations and reference reporters to detect M. tuberculosis from direct specimens (7).
In recent years, several clinical studies have been done about the specificity and sensitivity of IS6110 gene in the diagnosis of tuberculosis due to false positive or false negative reports with IS6110 primers. The use of molecular and sequencing methods is beneficial for the accurate and specific diagnosis of drug-resistant M. tuberculosis strains (8).
Culture method for mycobacterium is very long procedure and is not suitable for the rapid detection in the health centers and planning treatments for the patients. Therefore, it is not recommended by the directly observed treatment, short-course (DOTS) program.
It has been reported that this bacteria could get resistant to the first and second lines of drugs if not treated on time and would increase resistant to drugs (9).
The repetitive sequences of the IS6110 gene in the M. tuberculosis genome have been applied as an essential target for the PCR amplification. Several studies have been reported to evaluate the effect of the IS6110 sequence for the diagnosis of tuberculosis. In this study, we tried to do rapid detection of M. tuberculosis in the patients referring from several health centers and hospitals using IS6110 gene-based PCR test (10).
From 3012 clinical samples suspected to tuberculosis referred to the Masoud Laboratory from January 2019 to December 2021, 60 isolates were identified as MDR strains (resistant to at least isoniazid and rifampin or both of them) through the smear, culture, and antibiotic tests Then, by the IS6110 gene PCR, 54 (90%) samples were identified and confirmed as Tuberculosis and 6 (10%) as NTM.
Smear preparation and culture
The procedure was performed according to the CDC guidelines. After decontamination by the Petroff’s method, the slides were stained by the Ziehl–Neelsen stain, and mycobacterium bacilli were seen in all samples. They were cultured in two Lowenstein-Jensen media (11).
Antibiogram test of M. tuberculosis
Drug susceptibility testing (DST) was done by proportional method including isoniazid (0.2 gr/ml), rifampin (40 gr/ml), and ethambutol (2 gr/ml) to determine the resistance to drugs. M. tuberculosis H37Rv strain was used as the quality control (12).
DNA extraction and PCR reaction
To extract the whole genome, several colonies were transferred to microtubes containing sterile distilled water (200 μL), and placed in heat block instrument (98°C) for 60 min to inactivate and kill the microorganism. The DNA samples were extracted by Roche kit (Germany).
PCR reaction was performed in 25 µL volume including Master Mix, forward and reverse primers (Bioneer, Korea) (Table 1), extracted DNA, and deionized water. The cycling steps were as follow: initial denaturation (at 94°C for 5 min), 32 cycles of denaturation (at 94°C for 1:45 min), annealing (at 68°C for 1:45 min), and extension (at 72°C for 1:45 min), and a final extension at 72°C for 5 min. The PCR products were then run on 2% agarose gel and examined for the presence of the 123-bp and 209 bp bands after ethidium bromide staining. Three samples were detected positive and sequencing was conducted by Royan Biostiagen Company in order to confirm. The analysis of sequencing data was done by Chromas software (13).
Table 1. Primer sequences used for the IS6110 gene PCR (14)
| Sequence | Primers |
| 5′-CCTGCGAGCGTAGGCGTCGG-3′ | IS6110 F |
| 5′-CTCGTCCAGCGCCGCTTCGG-3′ | IS6110 R |
All samples consist of rifampin-resistant and MDR isolates were amplified with specific primers of the IS6110 gene. The H37RV was used as positive control for M. tuberculosis (Figure 2).
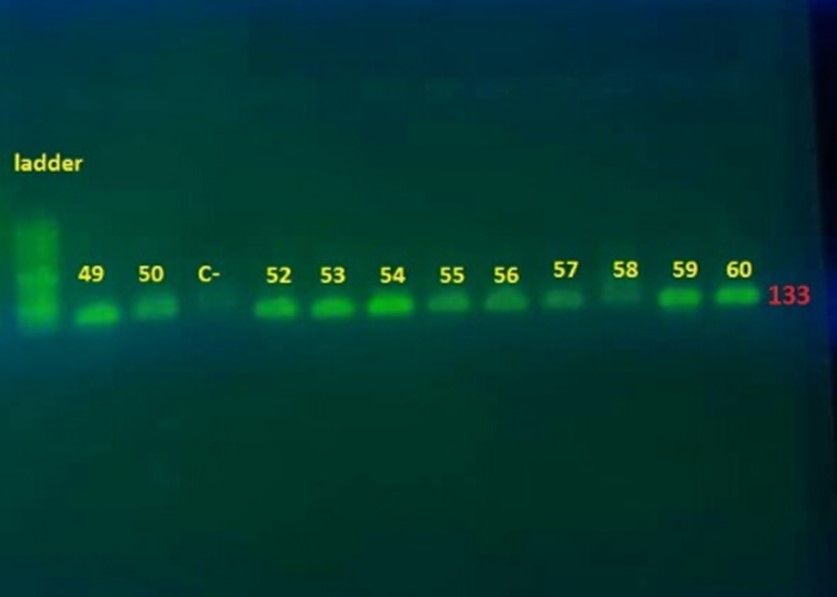
Figure 1. Gel image of IS6110 gene PCR results (133 bp), sample 60 is a positive control (H37Rv)
In 2007, Rouhani et al., from Kashan province showed that among 32 samples with positive PCR result, 30 samples (93.75%) and 22 samples (64.45%) were confirmed by culture and smear, respectively. Except for 6 samples, all with positive smear and positive culture results were positive for PCR (17). However, in our study, 100 samples (3.3%) were cultured positive.
In 2009, Javid et al., in Golestan province determined 87 cases of M. tuberculosis out of 104 positive culture samples as using IS6110 prime, 4 samples (3.8%) were obtained rifampin–resistant, and 2 samples (2.3%) were MDR (18). But, in our study, out of 54 M. tuberculosis samples, 3 (5%) were rifampin-resistant, and the others (94%) were MDR (18).
In 2012, Zaker et al., detected 207 isolates of M. tuberculosis by conventional phenotypic methods and specific PCR based on the IS6110 identification (19). In our study, 54 isolates belonging to M. tuberculosis were detected by conventional PCR based on the same gene.
The NAATs have been used for many years mostly in developed countries. Sensitivity of NAATs, using culture as a gold standard test, is 95% in the smear-positive patients and varies between 50–80% in the smear-negative patients. Hence, performing an accurate, quantitative, and sensitive M. tuberculosis detection is still a challenge (20).
Many questions remain concerning the effectiveness of NAATs for the smear-negative pulmonary and extrapulmonary TB in adults, detection of paucibacillary forms of TB (e.g. pediatric disease), and previously treated individuals. Furthermore, there is no universal test available and applicable to all patients (21).
In the past, epidemiological studies for tuberculosis were limited to available tools such as drug susceptibility profiles and phage-based typing, that both have limitations. In recent years, M. tuberculosis strains undergo minor and major genetic mutations during treatment and become resistant to the TB drugs. Molecular diagnostics have been improved in recent years (22).
In this clinical study, the IS6110 gene, one of the best markers for the differentiation of Mycobacterium complex, was used and suggested for the rapid detection in medical diagnosis laboratories. The molecular method is more sensitive and more accurate than the phenotypic method. The PCR-IS6110 process has a higher sensitivity and is known as the reference method to identify the resistant strains of M. tuberculosis from other atypical mycobacteria. It can also be used in molecular studies of tuberculosis to understand the pattern of genetic changes. Research work must continue towards developing advanced molecular techniques for the rapid and accurate diagnosis of TB with better performance characteristics that can be easily implemented for the routine TB diagnosis in the low-resource countries.
We would like to thank Masoud Laboratory’s Staff, Microbiology Unit, for their kind help in providing the data.
Ethical Considerations
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research and Ethics Committee of Islamic Azad University, North Tehran Branch. All methods were carried out in accordance with relevant guidelines and regulations.
Authors’ Contributions
All authors contributed equally to the preparation of this research article including, study concept and design, data collection, analysis and interpretation, and drafting and revision of the manuscript.
The author(s) received no financial support for the research or publication of this article.
Conflicts of Interest
Received: 2024/04/21 | Accepted: 2024/08/18 | ePublished: 2024/09/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |