BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-1872-en.html
2- Department of Virology, Faculty of Medicine, Iran University of Medical Science, Tehran, Iran
3- Department of Pediatrics, Erfan Niayesh Hospital, Tehran, Iran
4- Molecular Biology Research Center, Systems Biology and Poisonings Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran ,
In late 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused the Coronavirus disease 2019 (COVID-19) infection that developed into a pandemic infection in a short time. SARS-CoV-2 causes respiratory disease with a widespread collection of asymptomatic or mild to severe diseases (1-3). During the COVID-19 pandemic, children are less affected than adults, and underlying conditions and older age are associated with severe disease (4-6). Recently, following the SARS-CoV-2 pandemic, outbreaks of cases with Kawasaki-like disease (KLD) and a few others with the multisystem inflammatory syndrome in children related to COVID-19 (MIS-C) have been reported (7). A cohort study by Verdoni et al. in Italy showed that the SARS-CoV-2 epidemic increased the incidence of KLD (8). Also, Jones et al. reported a six-month-old baby with concurrency COVID-19 and KLD (9). Here, we report a pediatric case diagnosed with KLD associated with COVID-19 infection to highlight the clinical features and signs.
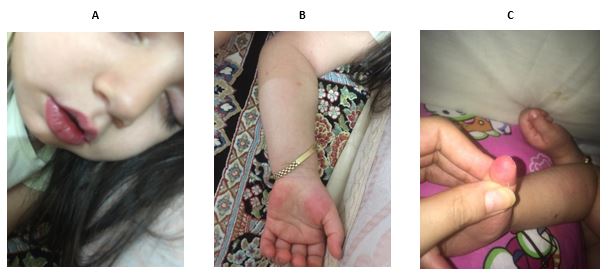
Figure 1. images of a child with concurrent COVID-19 and Kawasaki. The clinical signs of a child with Kawasaki can be seen in the following figures.
Clinical signs of a child with Kawasaki disease:
A: Swelling and redness of the lips
B: Skin rash on the palm of the hand
On the first day of hospitalization, a single dose of anti-inflammatory drug containing 2g/kg intravenous immunoglobulin IVIG and a high dose of acetylsalicylic acid (ASA 20 mg/kg four times daily) were administered. By the fifth day of hospitalization, skin rashes, swelling, and redness of the skin were observed, and the patient was agitated and lethargic. On the sixth day, the skin rash decreased, and the patient was not restless but lethargic. On the seventh day, the appetite returned, and 90% of the skin symptoms were improved. Laboratory tests for SARS-CoV-2 were positive. The patient was refreshed and discharged from the hospital on the eighth day. On the ninth day, all clinical symptoms improved, and only the scaling of the fingers began and lasted for about five days. The findings confirmed Coronavirus concurrent with Kawasaki.
The SARS-CoV-2 virus infection began in China in December 2019 and spread worldwide (10). The symptoms of COVID-19 are more severe in adults than in children (11). Because, in most cases, especially in children, COVID-19 is asymptomatic, they can transmit the virus to adults (12, 13). Several studies have reported concurrent infection with Kawasaki and COVID-19. However, to the best of our knowledge, it is one of the first reports of concurrent COVID-19 and KLD in Iran. KLD in children under five is associated with vasculitis and fever and is accompanied by skin rashes. The cause of Kawasaki syndrome is unknown. The important acceptable hypothesis supports an aberrant immune system response to unknown pathogens in genetically predisposed patients, but infectious agents such as viruses may be the triggers for this syndrome (14). Previous studies have shown that the prevalence of KLD increases in winter and spring (14). Respiratory infectious agents are considered one of the stimulants of this disease. Some studies reported up to 42% of Kawasaki syndrome after respiratory infections (15). Turnier et al. found that about a quarter (28%) of Kawasaki cases were attributed to rhinovirus and enterovirus infections. Parainfluenza and other respiratory viruses, such as respiratory syncytial virus (RSV) and Coronavirus, contribute less to the disease (15). Another study conducted by Cazzaniga et al. reported a KLD case associated with SARS-COV-2 and co-infection enterovirus and rhinovirus according to PCR tests. However, the cause of KLD was unclear due to the three viral agents that may be had been the trigger (16). Moreover, up to now, there are large case series of KD related to COVID-19 in different countries, e.g., the United Kingdom (UK), Italy, the United States of America (USA), Turkey, and France (16, 17) Similar to previous studies, in our case, fever and skin rash were the most important clinical symptoms, and after receiving the treatment, the clinical symptoms improved (17).
This case report could be helpful for clinicians caring for children with COVID-19 to identify new patterns of clinical signs of the disease. However, detecting clinical signs of COVID-19 in children requires extensive studies, and the disease appears to be related to Kawasaki.
None.
The head and manager of Erfan Hospital, Iran approved this study. All data were obtained from the routine clinical process.
"Written informed consent was obtained from the patient to publish this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Self-funding.
Conflicts of Interest
The authors report no conflicts of interest in this work.
Received: 2022/10/25 | Accepted: 2023/02/28 | ePublished: 2023/06/26
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








