BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-1601-en.html


 , Mojgan Minoo Sepehr2
, Mojgan Minoo Sepehr2 

 , Mohammad Reza Mozayan3
, Mohammad Reza Mozayan3 

 , Parisa Bagheri4
, Parisa Bagheri4 

 , Arefeh Dehghani5
, Arefeh Dehghani5 

 , Elham Rezaee6
, Elham Rezaee6 


2- Infectious Diseases Department of Yazd Health Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
3- General Courses Department, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
4- Department of Hematology and Blood Banking, Paramedical School, Gerash University of Medical Sciences, Gerash, Iran
5- Biostatics and Epidemiology Department, School of Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
6- Department of Medical Parasitology and Mycology, Faculty of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran ,
Malaria is one of the most serious life-threatening diseases in the world. It is also the leading cause of death in developing countries, especially in Africa. Approximately 86% of the cases occur in children (1) and it is one of the health problems in 95 countries of the world (2). This parasite is endemic to parts of Asia, Europe, and Africa. The disease is caused by protozoan parasites of the genus Plasmodium in humans. Four types of it are known to infect humans: Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, and Plasmodium ovale infection, with each species bearing different clinical results in patients. The most dangerous species of Plasmodium in the world is P. falciparum, although other species of Plasmodium can induce a severe type of disease in humans (3). Generally, more than 90% of deaths around the globe are attributed to Plasmodium falciparum (99% in Africa, mainly children under 5 years old) and 7.2% due to Plasmodium vivax (4). In Africa, the most common cause of Malaria in humans is P. falciparum, and P. vivax is the most common species in Southeast Asia (3). Approximately 3,500 species of mosquitoes have been identified worldwide, 60 species of which belong to the Anopheles genus that can transmit the Plasmodium parasite to humans (1, 5). Based on the latest WHO report released on 30 November 2020, there were 229 million malaria cases in 2019, with an estimated 409,000 deaths, compared to 228 million in 2018 with estimated deaths of 411,000 (6, 7). Scores of countries have made significant progress towards malaria elimination programs, with 33 countries reporting less than 1000 cases in 2015, while only 13 countries were estimated in 2000 (4, 5). Iran is one of the most malaria-endemic countries in the world so the total number of registered cases in 2015 appeared to be less than 200 cases; also, in 2016 and 2017, less than 90 and 89 cases of local population transmission were observed, which was more than four-fifths. Cases of the disease have been reported in Sistan and Baluchestan and Hormozgan provinces in the southeast and south of the country (8). The beneficial implementation of therapeutic and preventive control strategies through an appropriate healthcare system has led to this remarkable achievement (9). Iran began a malaria eradication effort in 2009 to achieve this by 2025. Since then, there has been tremendous progress, but the persistent possibility of malaria cases being imported from Pakistan and Afghanistan remains a significant political, social, operational, and technological hurdle to malaria eradication in Iran (10, 11). Imported Malaria may occur in travelers or military staff and immigrants from endemic countries entering the region. France is one of the first countries to detect imported malaria, with approximately 4,000- 5,000 cases detected each year (12). Yazd province and the historical city of Yazd have been known to be a 'world heritage'. This region is located in the center of Iran and enjoys a temperate climate. It is not a malaria-endemic area, but because it is very active in construction projects and is an industrial city, it hosts internal and foreign immigrants, as well as refugee workers from malaria-prone areas who may be in contact with malaria (1, 13). This survey aimed to find out the trend of malaria in Yazd, a central province of Iran in 2011-2020.
This descriptive-retrospective study was carried out to uncover the epidemiological characteristics of malaria in Yazd province. In general, the patients suspected of malaria, both Iranians and foreigners, all of whom were living in Yazd and had been referred to Yazd Central Health Service (CHS) from 2011 to 2020, were meticulously analyzed and reported. Demographic information of the individuals was recorded through a questionnaire (gender, nationality, age group, residence place, and type of human malaria parasite). This survey was approved by the Ethics Committee of the research group of Yazd University of Medical Sciences, with the ethics code: IR.SSU.MEDICINE.REC.1393.10. A drop of blood was first taken from the patient's middle finger with a sterile needle and placed on a clean slide to prepare a peripheral blood smear. It was spread with another slide, and then each slide was stained with Giemsa after fixation with methanol and examined with a light microscope by a skilled technician. Data were analyzed using SPSS18.
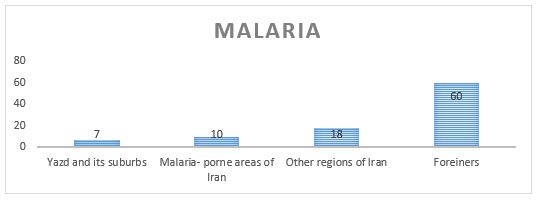
On the whole, 95 confirmed reported malaria patients were investigated from 2011 to 2020; 90 (94.7%) patients were male and 5(5.3%) were female (Chi-square, P=0.21). The mean age of the patients was 33.7 years for men and 21.4 years for women. Species of Plasmodium (L) falciparum was isolated from 81 cases (85.26%), but Plasmodium (p) vivax was isolated from 14 cases (14.74%). As Figure 1 illustrates, the highest rates of malarial disease were observed in 2013, 2015, and 2018 each with 15 cases (15.8%), but in 2017, there were only 5 cases (5.3%) (Chi-square test, P=0.021). Figure 2 displays the malaria cases predicted in the place of living (Yazd & suburbs, Malaria-prone areas of Iran, other regions of Iran, and foreigners), (Chi-square test, P=0.45).
Figure 1. Prevalence of Malaria according to year. Chi-square test, P<0.05.
Figure 2. Prevalence of Malaria according to the origin of life. (Chi-square test, P>0.45)
Table 1 reveals the prevalence of malaria according to age group. As shown in Table 1, the highest rate of Plasmodium (L) falciparum was seen in the 30-39 years age group with 27 cases (33.3%), and the lowest in the 05-19 years age group with 4 cases (4.94%). The highest rate of Plasmodium (p) vivax was observed in the 50≤ years age group with 6 cases (42.86%), and the lowest in the 05-19 and 20-29 years age groups with 1 case (7.14%), As Table 1 further indicates, the highest rate of mixed parasites of both, Plasmodium (L) falciparum and Plasmodium (p) vivax was seen in the 30-39 years age group with 29 cases (30.53%), but the lowest rate was observed in the 05-19 years age group with 5 cases (5.26%) (Chi-square test, P<0.021).
Table 1. Prevalence of imported malaria according to age groups.
| Age group | Plasmodium(L)falciparum Number Percent |
Plasmodium (P)vivax Number Percent |
Total Number Percent |
| 05-19 | 4 4.94% | 1 7.14% | 5 5.26% |
| 20-29 | 15 18.52% | 1 7.14% | 16 16.8% |
| 30-39 | 27 33.33% | 2 14.29% | 29 30.53% |
| 40-49 | 20 24.70% | 4 28.57% | 24 25.2% |
| 50≤ | 15 18.52% | 6 42.86% | 21 22.1% |
| Total | 81 100% | 14 100% | 95 100% |
Chi-square test, P<0.05.
Table 2 sets out the prevalence of malaria according to the geographical area. As Table 2 displays, the highest rate of malaria was observed in Yazd City with 49 cases (51.63%), but the lowest rate was seen in Meibod with 4 cases (4.2%). (Chi-square test, P=0.041).
Table 2. Prevalence of imported malaria according to the geographical area
| Geographical area | Malaria Number Percent |
| Yazd | 49 51.6% |
| Sadoogh | 14 14.7% |
| Mehriz | 10 10.5% |
| Ardakan | 6 6.3% |
| Taft | 6 6.3% |
| Abarkouh | 6 6.3% |
| Meibod | 4 4.2% |
| Total | 95 100% |
Chi-square test, P<0.05.
Figure 3 indicates the prevalence of malaria based on the job. As shown, the highest rate of the disease was identified with 69 cases (72.63%) in workers, but the lowest rate was observed with 4 cases in the farmers (4.21%) (Chi-square test, P=0.041).
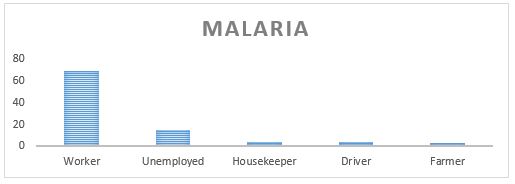
Figure 3. Prevalence of malaria according to the job (Chi-square test, P<0.05)
Malaria is one of the dominant causes of death in the world by imposing varying adverse effects on populations. It is a real menace in developing countries with more than 3000 deaths every day (14). Malaria has been widely prevalent in Iran for a long time, with a total risk of 2,714,648 persons with mainly 60% of this population living in endemic centers including Kerman, Hormozgan, as well as Sistan, and Baluchestan provinces; before starting any anti-malarial campaign, about 30 to 40% of the total mortality was due to malaria (15). Despite reports of high morbidity and death in previous decades, the current malaria condition in Iran demonstrates a victorious eradication in most divisions of the country. The malaria outbreak has been lowered from 333/1000 cases in 1921 to 0.01/1000 in 2017 (15). In our study, the overall of 95 confirmed reported malaria patients were investigated from 2011 to 2020; Of these, 90 (94.7%) were male and 5 (5.3%) were female. The mean age of the patients was 33.7 years for men and 21.4 years for women. Species of Plasmodium (L) falciparum were mainly isolated from 81 cases (85.26%), but Plasmodium (p) vivax was isolated from only 14 (14.74%) cases. The highest rate of malarial disease was identified in the years 2013, 2015, and 2018. The highest rate of Plasmodium (L) falciparum was observed in the 30-39 years age group with 27 cases (33.3%), but the lowest rate was seen in the 05-19 years age group with 4 cases (4.94%) as compared to 58.17% cases in Khan et al.'s study (16). The highest rate of Plasmodium (p) vivax was seen in the 50≤ years age group with 6 cases (42.86%), but the lowest rate was observed in the 05-19 and 20-29 years age groups with 1 case (7.14%) as compared to 40.81% in Khan et al.'s study (16). In our study, the prevalence of malaria was higher in men than in women; our result is in line with that of Khan et al., Sheikh et al., and Yang et al. (16-18). In this study, the highest rate of malaria was identified in the workers with 69 cases (72.63%), but the lowest in the farmers with 4 cases (4.21%); this is in line with the results of Yang et al. (18).
In this retrospective analysis of patients hospitalized with COVID-19 in the province of Khuzestan in southwestern Iran, we had several key findings: First, only one in seven patients presented to the hospital with an ambulance. Second, patients who presented with an ambulance had
Using the joint modeling approach, several demo-graphic and clinical factors were found to predict the EMS utilization and in-hospital
The authors would like to t
This research did no
The Ethics
The datasets used and/or analyzed d
Conception
Ethical approval to p
Conflicts of Interest
The authors declared no competing interests.
Received: 2022/01/9 | Accepted: 2022/07/13 | ePublished: 2023/01/20
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




.JPG)