BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijmm.ir/article-1-1081-en.html

 , Sakineh Hajebrahimi2
, Sakineh Hajebrahimi2 
 , Fatemeh Sadeghi-ghyassi1
, Fatemeh Sadeghi-ghyassi1 
 , Hadi Mostafaei3
, Hadi Mostafaei3 
 , Nasrin Abolhasanpour4
, Nasrin Abolhasanpour4 
 , Amirreza Nasseri4
, Amirreza Nasseri4 
 , Zahra Sheikhalipour5
, Zahra Sheikhalipour5 
 , Hanieh Salehi-Pourmehr6
, Hanieh Salehi-Pourmehr6 


2- Research Center for Evidence-based Medicine, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran | 4. Iranian Evidence Based Medicine Center of Excellence and Joanna Briggs Institute (JBI) of Australia, Vienna, Australia
3- Department of Urology, Comprehensive Cancer Center, Medical University of Vienna, Vienna, Austria
4- Research center for Evidence-based- medicine, Faculty of medicine, Tabriz University of Medical Sciences, Tabriz, Iran. 2. Iranian EBM Center: A Joanna Briggs Institute Affiliated Group.
5- Department of Medical Surgical Nursing, Tabriz University of Medical Sciences, Tabriz, Iran
6- 1. Research center for Evidence-based- medicine, Faculty of medicine, Tabriz University of Medical Sciences, Tabriz, Iran.2. Iranian EBM Center: A Joanna Briggs Institute Affiliated Group. ,
.
On December 31, 2019, Wuhan Municipal in Hubei Province, China, reported a cluster of pneumonia cases with unknown etiology and after one week a novel coronavirus was isolated from the patients; the virus was officially named by the WHO as “COVID-19”. The COVID-19 can spread through person-to-person transmission, droplets and aerosols. It was then approved that person-to-person transmission of COVID-19 happens more prominently in hospitals and the disease amplification occurs mostly in health centers (1, 2).
In the outbreak of infectious diseases, non-pharmacological interventions such as masks and respirators might be the only available protection tools. Since the outbreak of COVID-19, various tools have been used for health care and safety around the world including cotton or gas masks, medical or surgical masks and respirators such as N95, N99, N100, P2, P3, FFP2 and FFP3 which differ based on their design and indication of use (3-5). Some countries like Singapore, did not recommend healthy people to use masks but in neighboring Malaysia and Thailand, the government urged people to always have masks ready. Conflicting messages have showed confusion over how to protect against COVID-19 (6).
One of the useful experiences learned from Severe Acute Respiratory Syndrome (SARS) contagion was detecting the protective role of wearing masks against SARS and other viral infections. WHO considers using hand hygiene and masks as preventive measures to limit the spread of COVID-19 in infected areas (7). Therefore, this systematic review aims to investigate whether it is or is not necessary to wear masks in coronavirus outbreaks in the community.
This systematic review and meta-analysis is conducted based on the Cochrane Collaboration Handbook and PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (14). Databases including PubMed, Embase, Medline (via Ovid), Cochrane library, Up-To-Date, WHO, TRIP database and Google Scholar were searched on February 28, 2020, to find possible related evidence. For this purpose, the following keywords were searched: "COVID-19"; "COVID 19"; 2019-nCoV; 2019-CoV; coronavirus; mask* and facemask. We updated the search in March 13, 2020.
The search strategy was set to each database and proper keywords were searched when possible. A total of 982 relevant reports were identified after removing duplicates. Of these, 71 references were screened based on titles and abstracts. After excluding unrelated studies, 36 studies were included in the full-text review and were assessed for eligibility. Finally, a retrospective study and a case series study met our inclusion criteria for data extraction. Also we updated the search at March 13, 2020 for any more relevant papers. In this stage we found 140 more studies, in which after screening, only one study met our inclusion criteria and was added to our result (Figure 1).
Mask Protection from COVID-19 in Healthcare Setting and Community
Wang et al. (8) retrospectively collected infection data in the time interval between January 2 to January 22, 2020, in six different departments (Lung, ICU, Infection, Pancreatic Hepatobiliary Surgery, Trauma, Microsurgery, and Urology) from Zhongnan Hospital of Wuhan University. Health care providers of respiratory, ICU and infectious diseases department who used N95 respirators, disinfectants and frequently hand cleansers, were enrolled in the study as “the N95 group”. Given the lack of awareness of COVID-19 in the early days of the outbreak, medical staff in the other three wards of the hospital did not use any medical masks and occasionally used disinfectants and hand hygiene. This group was considered “the no-mask group”. The cases suspected to COVID-19 infection were diagnosed with chest CT and were confirmed by molecular diagnostic methods. Of the total patients, 28 confirmed and 58 suspected cases were diagnosed during the study data collection period. Medical staff contact with COVID-19 patients in the N95 group was significantly greater than in the no-mask group (for patients confirmed: difference: 733; odds ratio: 8.33).
The results of Wang et al. showed that of 493 medical staff, there were no cases of infection among nurses (222) or physicians (56) in the N95 group. In the no-mask group, the infection was observed in 10 medical staff (out of a total of 77 physicians and 136 nurses) (8). Regardless of the high level of exposure to the COVID-19 virus in the N95 group, the infection rate in medical staff in the group using this mask was lower than that of the group that did not use the mask. (Difference: 4.65%, (95% CI: 1.75%-infinite)) (Adjusted odds ratio (OR): 464.82, (95% CI: 97.73-infinite)). This study was not peer-reviewed and therefore the level of evidence was low.
In another study carried out by Chan et al., (9) epidemiological, clinical, laboratory, radiological and microbiological findings as well as phylogenetic properties were analyzed in six family members (four adults and two children) with symptoms of unexplained pneumonia who had travelled from Shenzhen, Guangdong Province to Wuhan, as well as another family member who did not travel to Wuhan (7 family members in total).
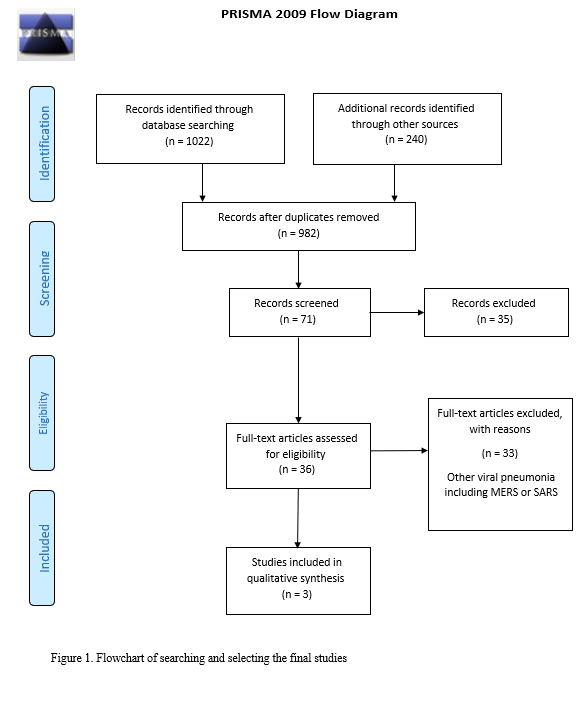
Figure 1
A study in Hong Kong society in the first 42 days after announcement of a cluster of pneumonia in China, could maintain zero nosocomial transmission of COVID-19 since the importation of first confirmed case since day 22. Eleven of 413 healthcare workers caring patients before confirmation of COVID-19, had unprotected exposure with confirmed cases and none of them was infected. Also, they couldn’t detect RNA of virus in 8 air samples collected at a distance of 10cm of patient’s chin. This suggested COVID-19 is not transmitted by airborne route, whether the conclusion based on analysis of one patient is not reliable. It can also be because of rapid dilution of air inside airborne infection isolation room, or airborne route, too. Anyway, nosocomial transmission of COVID-19 was not observed and according to the results of this study, wearing surgical mask alone was not associated with protection of person from acquisition of COVID-19 (10).
Mask Protection in the Other Corona Viral Infections in Community Settings
Due to the newness of the COVID-19 virus, no clinical trial was found on the efficacy of different types of masks in preventing the disease among health workers or in community settings. However, several randomized clinical trials (RCTs) have been performed using the mask in line with extensive interventions (such as mask and handwashing) in the community and therapeutic centers and showed various outcomes in preventing transmission in occasional outbreaks of infectious diseases, like influenza.
Among the nine clinical trials that used the mask in the community settings, all studies except for one used the mask for respiratory protection. They found that using the mask alone and mask in addition to hand hygiene may be beneficial for protection from infection in community settings, indeed, if used early and adhered (11-19). However, the total level of evidence available to determine the effectiveness and efficiency of the mask alone is low to moderate due to the use of complex interventions.
Mask Protection in the Other Corona Viral Infections in Health Care Settings
We found four RCTs reporting the clinical efficacy of using masks or respirators among healthcare staff (20-23). The first RCT was conducted on 32 health workers in Japan. Health care providers were divided into two groups; a group using the medical mask and a control group. There was no significant difference in the occurrence of respiratory diseases between the two groups (P=0.81) (20).
Table 1. Summery of studies characteristics included in systematic review.
| Reference | Population | Mask type | Infected with mask | Infected without mask |
| Wang et al. (8) | 706 medical staff | N95 | None of 493 | 10 of 213 |
| Chan et al., (13) | 6 family members | surgical mask | None of 1 | 5 of 5 |
| Cheng et al., (14) | 11 healthcare workers | Surgical mask | None of 402 | None of 11 |
The third trial conducted on 1922 Chinese healthcare workers, compared the outcome in three groups including the use of the medical mask, use of the N95 respirator and a control group. N95 respirator had a protective role against clinical respiratory infections (odds ratio: 0.38, 0.17 to 0.86); however, it did not resist PCR-confirmed influenza. The overall results showed that since the highest infection rate was in the control group, the N95 respirator users observed a low infection rate .(22)
The fourth RCT was performed on 1669 health care workers in China to investigate the consequences of continued use of the N95 respirators and medical masks during high-risk procedures. The results of this study showed that the N95 respirator is very useful against clinical respiratory infections (hazard ratio: 0.39, 0.21 to 0.71) and bacterial colonization (hazard ratio: 0.40, 0.21 to 0.73) (23).
Any severe acute respiratory infections (SARI) among emergency medical staff require urgent examinations. Early diagnosis of SARI symptoms with unknown causes in medical treatment centers through a rapid triage and isolation system for suspected or confirmed COVID-19 infections has been strongly recommended to prevent and control the infection (25-27). Medical and cloth masks have been designed to prevent the person wearing the mask from spreading the infection and to protect the person from being contaminated through the blood or body fluids of patients. Furthermore, the respirator is a useful option to protect the person against respiratory infection (3-5).
The results of the present study showed that N95 respirator, with respect to hand hygiene and the use of disinfectants can reduce the incidence of COVID-19 in health care providers and in the other study, the use of medical mask decreased the rate of infection in one 7 years old child. A model study suggested that using the mask in the community may delay the pandemic outbreak of infection, although efficacy estimates were not based on clinical trial (28).
For people with no respiratory symptoms, medical masks are not required in the community, even if COVID-19 was an outbreak in the area. However, wearing masks is recommended in crowded environments (such as public transport) and for the high-risk individuals (elderly, pregnant women and people with underlying diseases). The use of masks does not diminish the importance of other public measures to prevent infections and may lead to unnecessary costs and provisions (29).
Lee et al. demonstrated that due to the unknown nature of the COVID-19 virus and insufficient knowledge of its transmission, hand washing and hygiene together with the use of eye protection and masks are protective recommendations for all health care providers (30). However, the extra demand for preparing a mask sometimes is a serious concern among the general public. Many people go to the pharmacy to purchase masks, which leads to decreased medical facilities in the emergency care centers (31).
In previous studies on investigation of Middle East Respiratory Syndrome-Coronavirus (MERS-CoV) Infection, it was recommended that wearing medical mask is necessary only in close contact (1 meter) and when health workers enter the room of patients (32). However, Xu et al. demonstrated that the most important material of novel coronavirus is the RNA that controls its replication and metabolism. The RNA strands are light, thus can freely float in the air and cause infection through contamination. Therefore, filtering gas mask can be beneficial tools to remove the novel coronavirus RNA strands that are connected to droplets and dust, but not for filtering the free RNAs in the air. They recommended isolated gas masks to hospital personnel that are in direct contact with patients (33). A study of immediate psychological responses during the Initial stage of COVID-19, found that wearing respirators, was associated with lower levels of depression and anxiety in society. Although the WHO emphasizes that masks are effective only when used in combination of hand hygiene, wearing a mask could offer potential psychological benefits by offering a sense of security (34). Despite the reported psychological benefits, using mask can be harmful too; because the low level of anxiety can lower society attention to healthcare system recommendations like hand hygiene and quarantine.
The results of the present study showed that respirator N95, with respect to hand hygiene and use of disinfectants can reduce the incidence of COVID-19 in health care providers and in another study, the use of medical mask reduced the rate of infection. Due to the newness of the COVID-19 virus, no clinical trials have been found regarding the use of the mask in the prevention of the disease. However, using masks in different community settings can protect if used early and on time. For health care providers, evidence suggests that respirators are more beneficial than masks during the epidemics and outbreaks. Respirators are also recommended if the disease is severe and when mortality is high and no medication or vaccine is available.
Strategy and guidelines for mask use in the entire world are inconsistent; possibly reflecting the relatively low number of RCTs available. Ultimately, the biggest priority is to provide evidence-based options to health care providers who need to be confident about their health and occupational safety and to ensure the integrity of an effective response to the epidemic.
Noun
Authors declared no conflict of interests.
- In the outbreak of infectious diseases, non-pharmacological interventions such as masks and respirators might be the only available protection tools.
- N95 respirator, with respect to hand hygiene and the use of disinfectants, can reduce the incidence of COVID-19 in health care providers.
- World Health Organization recommended that for people with no respiratory symptoms, medical masks are not required in the community.
- Wearing masks is recommended in crowded environments (such as public transport) and for the high-risk individuals (elderly, pregnant women and people with underlying diseases).
Received: 2020/03/22 | Accepted: 2020/03/29 | ePublished: 2020/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |